Next Lesson - Pneumothorax and Pleural Effusion
Abstract
- Tuberculosis (TB) is a chronic, communicable disease, caused by the bacteria Mycobacterium tuberculosis.
- TB is transmitted via droplet transmission, and an infective dose is between 1 and 10 bacilli, meaning the amount needed to infect another person is small.
- The initial TB infection with creation of the tubercle occurs on the first exposure to Mycobacterium tuberculosis. When the bacilli then deposit in the alveoli, there is usually the development of a primary or Ghon’s focus, a sub-pleural group of these tubercles, which can occur in any lung zone.
- TB has a gradual onset. Symptoms of pulmonary TB include tiredness, weight loss, fever (possibly with sweats) and a cough (dry or productive).
- Two different tests can be used to establish whether someone has been infected with TB: the QuantiFERON test or the Tuberculin skin test. These tests do not distinguish latent infection from active disease.
- Tuberculosis is treated through a long course of several antibiotics.
Core
Tuberculosis (TB) is a chronic, communicable disease, caused by the bacteria Mycobacterium tuberculosis. TB is common in areas like Africa, Asia and Latin America. It is uncommon in the UK, but the highest incidences occur in patients who have emigrated to the UK from a high risk area.
Mycobacterium tuberculosis is an aerobic organism that has a very unusual waxy component to its cell membrane, meaning that it cannot be reliably Gram stained. This means that Ziehl-Neelsen staining is the best mechanism for visualisation, taking between 2-6 weeks to culture. Due to the result of the Ziehl-Neelsen staining, Mycobacterium tuberculosis is known as an acid-fast bacilli.

Image - Mycobacterium tuberculosis as imaged using the Ziehl-Neelsen staining method
Public Domain Source by Public Health Image Library [Public domain]
TB is transmitted via droplet transmission, and only a small number of bacilli may be required to establish infection, depending on host and environmental factors.
Once the bacilli are inhaled by the body, alveolar macrophages engulf the bacterial deposits in alveoli, but are unable to kill them through the normal release of lysosomes, due to their specialised cell wall.
The macrophages initiate cell-mediated immunity. The release of Interferon-γ by the cell mediated immune system allows further activation of macrophages, which release reactive oxygen species (ROS) to try to kill the bacteria, and cytokines to promote an inflammatory response. These macrophages are now known as epithelioid macrophages (which are just macrophages that look like epithelial cells on microscopy). Some of the macrophages fuse, to form Langhans giant cells (multiple epithelioid macrophages fused together, with the nuclei arranged in a horseshoe)
The ingestion of the tuberculosis bacterium by epithelioid macrophages causes a granulomatous reaction, because even with the adaptations and the recruitment of the cell mediated immune system (T lymphocytes) the bacteria is resistant. This forms a tubercle, a spherical granuloma with central caseation. Under the microscope you are able to see caseous necrosis, epithelioid macrophages, Langhans giant cells and lymphocytes in a TB granuloma.

Image - Two Langhans giant cells marked by the green arrows. Note the horseshoe of nuclei
Creative commons source by Humpath, edited by Dr. Maddie Swannack [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The initial TB infection with creation of the tubercle occurs on the first exposure to Mycobacterium tuberculosis. When the bacilli then deposits in the alveoli, there is usually the development of a primary or Ghon’s focus, a sub-pleural group of these tubercles, which can occur in any lung zone.
The bacilli then drain from the primary focus into the hilar lymph nodes. The combination of the hilar lymph nodes and the primary focus is together known as the primary complex.
To recap:
- Tubercle - a spherical granuloma with central cessation, caused by the macrophages ingesting Mycobacterium tuberculosis.
- Primary/Ghon’s Focus - a sub-pleural collection of tubercles, which can occur in any lung field after initial TB exposure.
- Primary Complex - the primary focus plus the hilar lymph nodes into which the bacilli drain.
Most TB infections at this stage will heal, either with or without calcification of the primary complex.
However, in most people, before healing can occur some TB bacilli will enter the bloodstream via the lymphatic drainage, resulting in haematogenous spread of the bacilli to other parts of the lung and other organs. However, as the patient has developed cell mediated immunity against Mycobacterium tuberculosis, they will remain asymptomatic and the infection will be contained. This state can continue for years, or even for the rest of the patient’s life.
This phase, when the patient has the infection present but no symptoms of active disease, is known as latent tuberculosis. The person will remain well, but the potential for reactivation at any site is always present. Reactivation usually occurs when the host’s immune response is impaired, for example by infection with HIV, a haematological malignancy, prolonged immunotherapy, or substance abuse. At this point, the epithelioid macrophages containing the bacilli will fail, and the bacilli will spread, causing active infection again.
Latent TB Those initially infected with TB have around a 1 in 10 chance of developing active disease at some point in their life, either through the development of primary TB at the initial time of infection, or due to reactivation of latent TB following initial infection.
Primary TB occurs when the primary complex doesn’t heal, but instead progresses to active TB. The pathology seen in primary TB is similar to the pathology in reactivation of latent TB.
Reactivation of latent TB occurs most often in the lungs, most commonly in the upper lung zones due to the higher pO2 encouraging activation.
The following sequelae occur after activation through either mechanism:
- Cavity Formation - the caseous material undergoes liquefaction, and is then discharged into a bronchus. This causes the patient to cough up the material as thick phlegm. Fibrous tissue forms around the necrotic tubercle in an attempt to limit the rupture of tubercles and spread of bacilli, but isn’t usually successful.
- Haemorrhage - the necrosis spreads into vessels in the cavity walls, causing haemorrhage into the tubercle.
- Involvement of the Rest of the Lung - once a tubercle ruptures into the bronchi, infected material spreads the infection through the bronchial tree and into other lung zones.
- Pleural Effusion - a collection of fluid in the pleural space caused by either the presence of bacilli in the pleura or a hypersensitivity reaction, both of which cause inflammation.
- Miliary Tuberculosis - this occurs when a focus ruptures into a blood vessel, causing widespread dissemination of bacilli throughout the body, meaning that there is the formation of multiple ‘miliary’ foci in the lung and other organs, such as the brain (causing tuberculosis meningitis), spleen or pancreas.
Extra-pulmonary tuberculosis occurs when there is reactivation of latent TB in sites other than the lungs, resulting in active TB (note the difference between miliary TB, in which there is widespread active infection but it started in the lungs). Common sites include lymph nodes, bones, joints, the central nervous system, GI tract and urinary tract. This can cause a wide variety of symptoms depending on which organ systems are affected.
TB has a gradual onset, and symptoms of pulmonary TB include:
- Tiredness
- Weight loss
- Fever (possibly with sweats)
- Cough - dry or productive
There may also be haemoptysis due to the haemorrhage discussed earlier, but this will not happen in every patient.
There may be crackles on auscultation, but there may also be no clinical signs present, meaning a chest radiograph is essential in establishing a diagnosis. If there is fibrosis or a pleural effusion present, then clinical signs of these may be apparent.
A diagnosis of TB is more likely, and should therefore be considered, in people who were born outside of the UK, have a recent travel history to an area where TB is common, are immunocompromised, or have been in close contact with someone with TB.
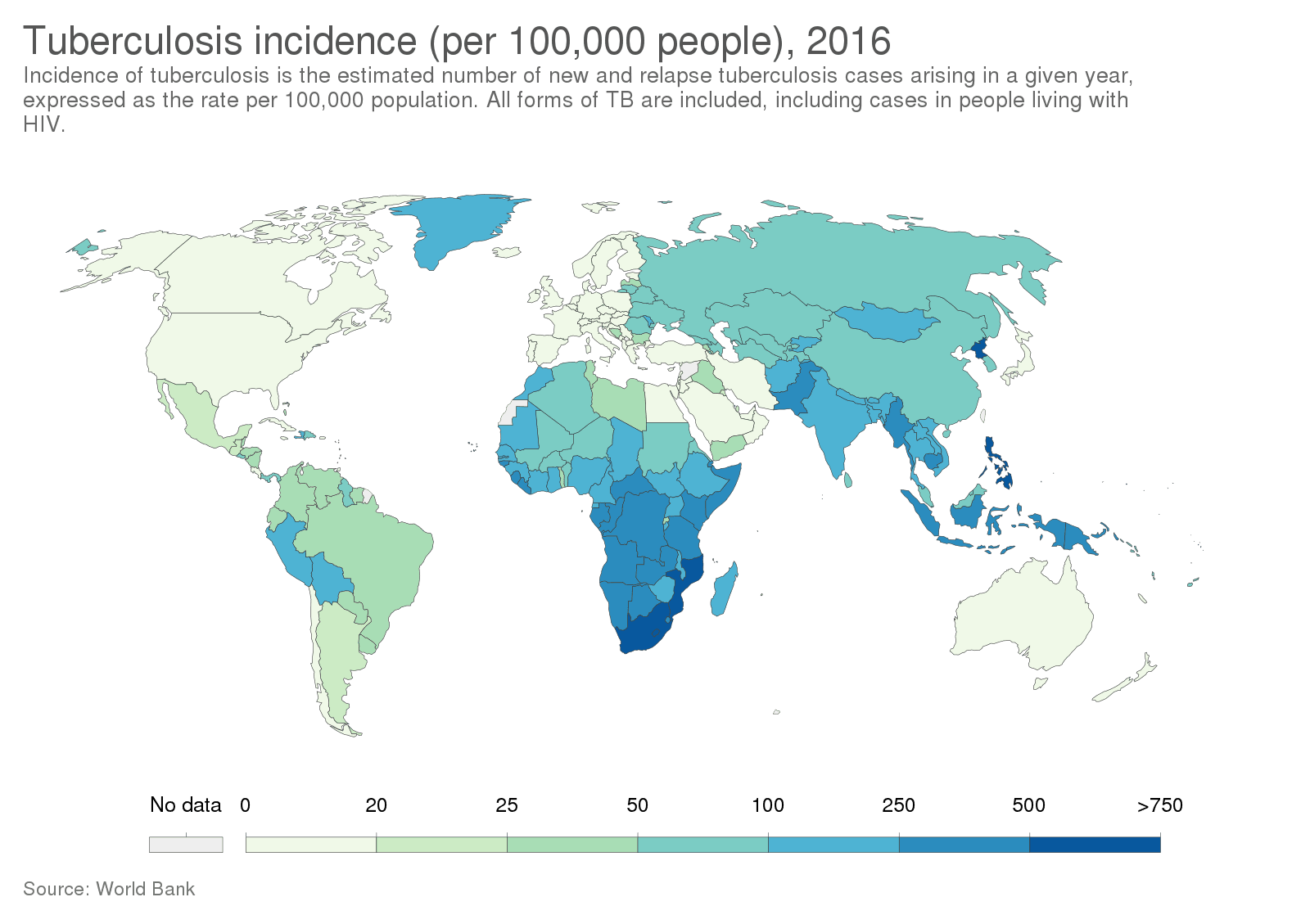
Diagram - The incidence (new cases in a year) of tuberculosis in 2016. The darker the blue, the more cases in that region. This information can be helpful when determining if a patient is at high risk of contact with TB
Creative commons source by Our World In Data [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Two different tests can be used to establish whether someone has a latent TB infection: the QuantiFERON test or the Tuberculin skin test.
- The QuantiFERON test is based on the ability of Mycobacterium tuberculosis antigens to stimulate the host production of interferon gamma from T Lymphocytes.
- A blood sample is taken from the patient, and their lymphocytes are then cultured with antigens of Mycobacterium tuberculosis. If a patient has been exposed to TB before, T lymphocytes will produce interferon gamma in response.
- The antigens used in this test are not present in the TB vaccine and are absent from most non-tuberculous mycobacteria, meaning that the QuantiFERON test can usually be used to distinguish latent TB from prior BCG vaccination or infection with atypical organisms.
- In the Tuberculin or Mantoux skin test, tuberculin, a protein derived from mycobacteria, is injected intradermally.
- If the patient has been previously exposed to TB there will be a type IV hypersensitivity reaction at the injection site between 48-72 hours after the injection.
- However, this test can result in a number of false results: false positives can be gained if the patient has had a previous BCG vaccine or if they have been infected with a non-tuberculous mycobacterium in the past (an atypical organism).
- False negatives can also occur if a patient is immunocompromised, as this may affect their ability to mount the hypersensitivity response.

Image - Administration of the tuberculin skin test
Public Domain Source by Centers for Disease Control and Prevention, Greg Knobloch [Public domain]
On a chest radiograph there will be shadowing, which may be in the form of patchy solid lesions, cavitated solid lesions, or streaky fibrotic flecks of calcification.

Image - Chest radiograph showing the shadowing seen in primary pulmonary TB. It shows the inflammation contained to one area (the right lower and middle lobes)
Creative commons source by "The Radiological Diagnosis of Pulmonary Tuberculosis (TB) in Primary Care". Journal of Family Medicine and Disease Prevention 4, Basem Abbas Al Ubaidi [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]

Image - Miliary TB, when the Mycobacterium tuberculosis has spread throughout the lungs (shown by the hazy appearance across all lung fields) due to spread through a blood vessel
Creative commons source by James Heilman, MD [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
However, a definitive diagnosis is established by the identification of the bacillus in sputum culture. In extra-pulmonary TB, investigations such as endoscopy, lumbar puncture or MRI may be indicated.
Tuberculosis is treated through a long course of several antibiotics. At the time of writing this article the recommended antibiotic treatment is:
- Rifampicin (6 months)
- Isoniazid (6 months)
- Pyrazinamide (2 months)
- Ethambutol (2 months)
The four drugs should be taken at the same time, taking all four for the first two months and then the rifampicin and isoniazid for a further four months. This combination therapy is used to prevent the increase of antibiotic-resistant strains, and to negate the effect of already resistant strains, as it is unlikely that the infection will be resistant to all four drugs.
These drugs have a wide array of severe side effects (this is just a selection):
- Rifampicin can cause hepatitis, orange colouring to the secretions (e.g. urine, tears), thrombocytopaenic rash (rash due to low platelet count), and failure of the COCP due to induction of the liver enzymes that normally metabolise it.
- Isoniazid can cause hepatitis, peripheral neuropathy and psychosis.
- Pyrazinamide can cause hepatitis, gout and arthralgia (pain in the joints).
- Ethambutol can cause optic neuritis and blindness.
This means that medical management of side effects is common: for example, vitamin B6 should be taken with isoniazid to prevent peripheral nerve damage.
The infectivity of sputum often becomes minimal after two weeks of commencing effective treatment in drug-susceptible pulmonary TB, meaning the patient is usually less infective to others, but the course must be finished to eradicate the disease in infected people.
Edited by: Dr. Maddie Swannack
Reviewed by: Dr. Thomas Burnell
- 6652

