Next Lesson - Anatomy and Physiology of the Hindgut
Abstract
- The midgut is defined as the section of the gut from the second part of the duodenum to two-thirds of the way along the transverse colon.
- It includes the duodenum, jejunum, ileum, caecum, appendix and transverse colon.
- The midgut only has a dorsal mesentery.
- Its arterial blood supply is by the superior mesenteric artery (SMA), its venous drainage by the superior mesenteric vein (SMV), with sympathetic fibres via the thoracic splanchnic nerves and parasympathetic innervation via the vagus nerve.
Core
Anatomical Features of the Intestines
The brush border refers to the microvilli on the apical surface of enterocytes in the small intestine, which increase surface area for absorption. Surface area is also increased by plicae circularis and villi.
- The first is the plicae circularis (see below), the mucosal folds of the wall of the small intestine.
- These are lined with villi, finger-like projections into the lumen that increase the surface area.
- On the surface of the villi cells are microscopic projections called microvilli. Each epithelial cell has many microvilli.
The brush is made up of a range of cells including: enterocytes (absorption), goblet cells (mucus production), enteroendocrine cells (hormone production), Paneth cells (antimicrobial peptide production) and stem cells (provide replacement of a variety of cell types). Enterocytes are the cells responsible for the majority of absorption.
The plicae circularis, also known as valvulae conniventes, are the circular folds in the walls of the small intestine. Unlike rugae in the stomach, they do not disappear when the intestine extends.
They slow the passage of the food through the intestine and provide a larger surface area for absorption.
Plicae circularis can be differentiated from haustra (found in the large bowel) because they cross the whole width of the bowel.
The large bowel has longitudinal ribbons of smooth muscle on the external surface called taenia coli. These fibres contract lengthways across the bowel, forming outpouchings of colon called haustra. The haustra can be differentiated from plicae circularis due to the fact they do not traverse the whole diameter of the bowel.
Vasa recta are straight arterial branches travelling within the mesenteries of the jejunum and ileum. They branch from the arcades, which are themselves anastomoses of the jejunal and ileal arteries.
In the jejunum, the vasa recta are few and long, whereas in the ileum they are shorter and more numerous.
The duodenum is the most proximal part of the small intestine. It is the section of the gut between the pylorus of the stomach and the start of the jejunum, and it is split into 4 parts.
The function of the duodenum is to neutralise the acidic chyme from the stomach with HCO3- rich secretion before it enters the jejunum. It is also where iron is absorbed from the chyme.
The Ampulla of Vater is located in the second part of the duodenum. This is where bile and pancreatic enzymes enter the small intestine from the biliary system, which are required for digestion of fat and proteins found in the chyme.
The duodenum has a dual blood supply from the gastroduodenal artery (a branch of the coeliac trunk) and the inferior pancreaticoduodenal artery (a branch of the superior mesenteric artery). Its venous drainage is into the veins of the same name, which then drain directly into the portal vein. Lymphatic drainage is into the pancreatoduodenal and superior mesenteric nodes.
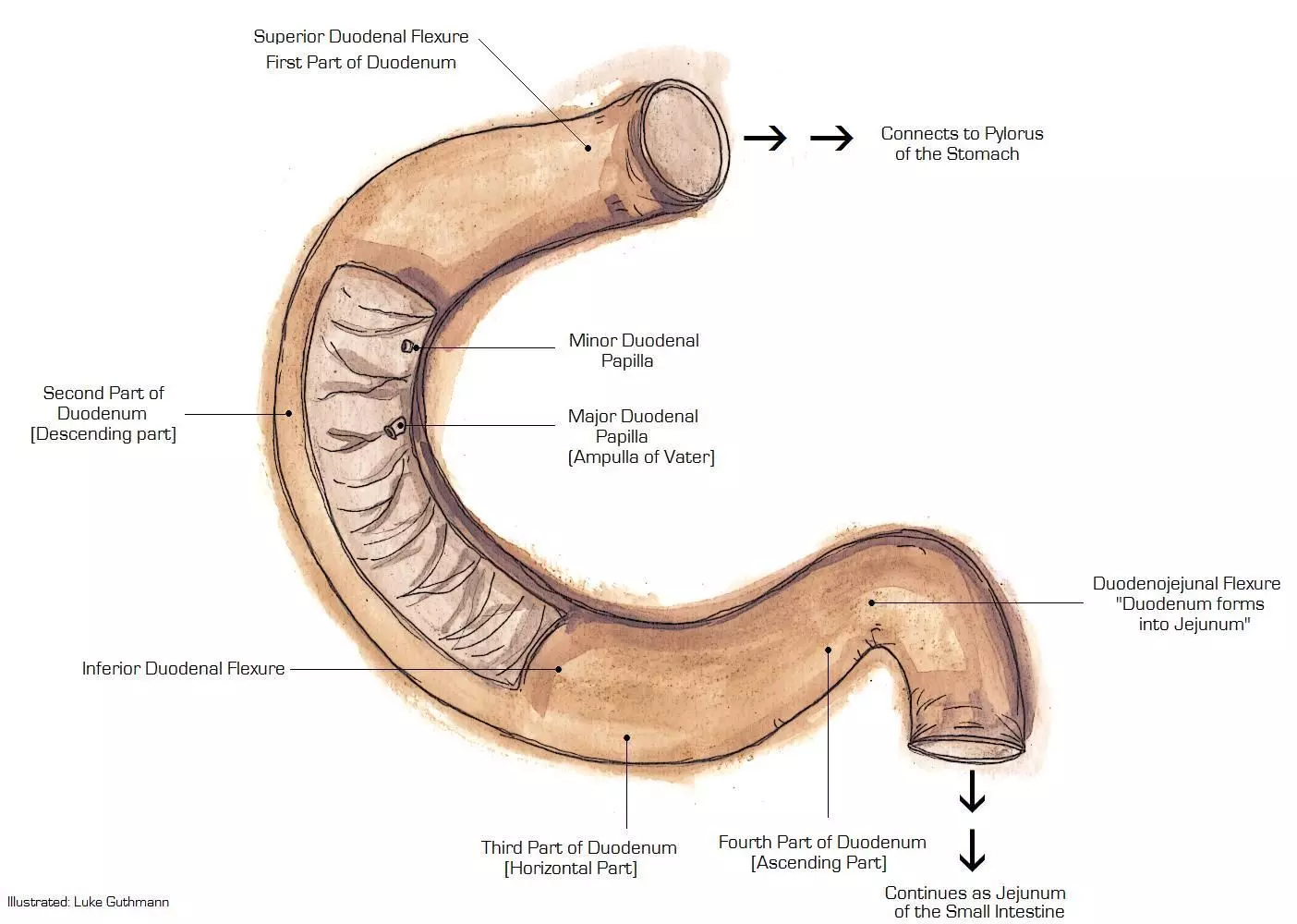
Diagram - The anatomy of the duodenum
Creative commons source by Luke Guthmann [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The jejunum is the second part of the small intestine. It begins at the duodenojejunal flexure and there is no clear anatomical landmark that marks where the jejunum ends, and the ileum begins. The jejunum is located in the left upper quadrant of the abdomen. It has a thick intestinal wall (due to an increased number of plicae circulares), long vasa recta and few arcades, and it is these features that differentiate the jejunum from the ileum.
The function of the jejunum is to absorb the majority of nutrients such as sugars, amino acids, and fatty acids. The jejunum is specifically designed for this function as the combination of plicae circulares, villi and microvilli (brush border) provide a very large surface area ideal for absorption.
The majority of absorption in the small intestine occurs within enterocytes in the brush border.
Monosaccharides are transported into enterocytes by transporters: SGLT1 absorbs glucose or galactose and GLUT5 absorbs fructose. These sugars are then transported across the basolateral membrane into the blood by GLUT2 (all monosaccharides). Enterocytes also absorb amino acids (as well as short peptides that have not been completely digested prior to absorption) via the PepT1 transporter.
The jejunum’s blood supply is from the jejunal arteries which branch off the superior mesenteric artery (SMA), and its venous drainage is into the jejunal veins which then drain into the superior mesenteric vein (SMV). Lymphatic drainage is into the superior mesenteric nodes.
The ileum is the third part of the small intestine and as previously stated it has no clear demarcation of where it begins. However, it ends at the ileocaecal junction where small bowel is connected to large bowel. The ileocaecal valve is located here to prevent reflux from the caecum back into the small intestine.
The ileum is mainly located in the right lower quadrant of the abdomen. It has thinner intestinal walls, shorter vasa recta, and more arcades than the jejunum.
The function of the ileum is to absorb the remaining nutrients not absorbed in the jejunum, including vitamin B12 and bile acids. It is also responsible for the absorption of a large proportion of the total water and electrolytes absorbed in the gut as a whole.
Water is absorbed in the small intestine through an osmotic gradient: sodium is co-transported with glucose and amino acids into the enterocytes, creating an osmotic gradient that water follows. Secretion of water into the intestine is predominantly driven by the movement of chloride ions.
The ileum’s blood supply is from the ileal arteries which branch off the SMA, and its venous drainage is into the ileal veins which then drain into the SMV. Lymphatic drainage is into the superior mesenteric nodes.
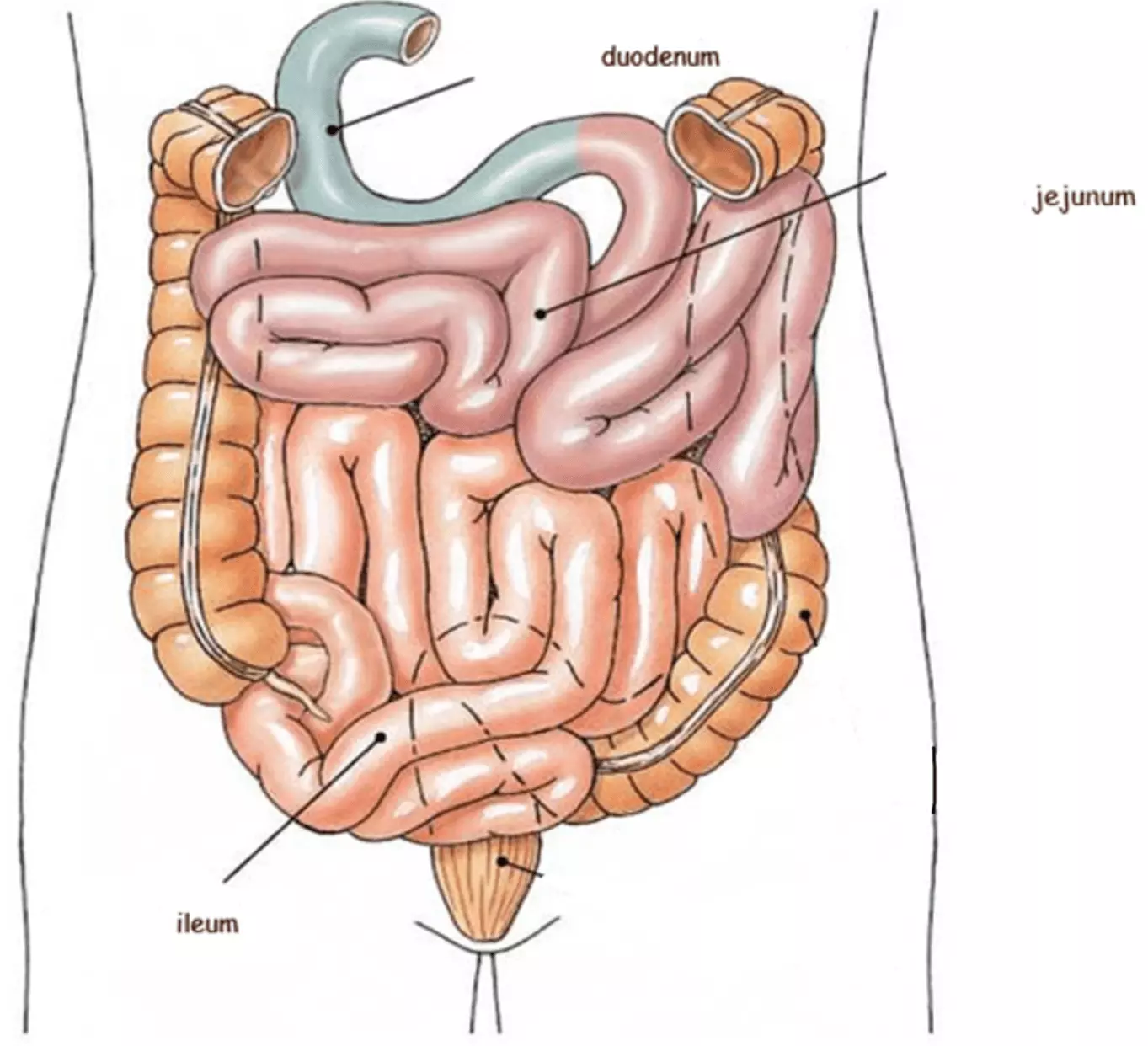
Diagram - The three divisions of the small intestine
Creative commons source by Vedzitux, edited by Dr. Laura Hansell [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The appendix is a narrow blind-ended tube that usually originates from the posteromedial aspect of the caecum. It is suspended from the terminal ileum by the mesoappendix (a section of mesentery). The position of the free end of the appendix can vary greatly, but its most common position is retrocaecal.
The arterial blood supply of the appendix is from the appendicular artery which is a branch of the ileo-colic artery, and its venous drainage is via the appendicular vein which drains into the SMV. Lymphatic drainage is into the ileo-colic lymph nodes. The appendicular artery, vein, and lymphatics lie within the mesoappendix.
The appendix has no essential functions in the body, although it contains lymphoid tissue and is thought to have a role in immune function. Because it is a blind-end pouch it is a site predisposed to collections, which can become inflamed or infected, called appendicitis.
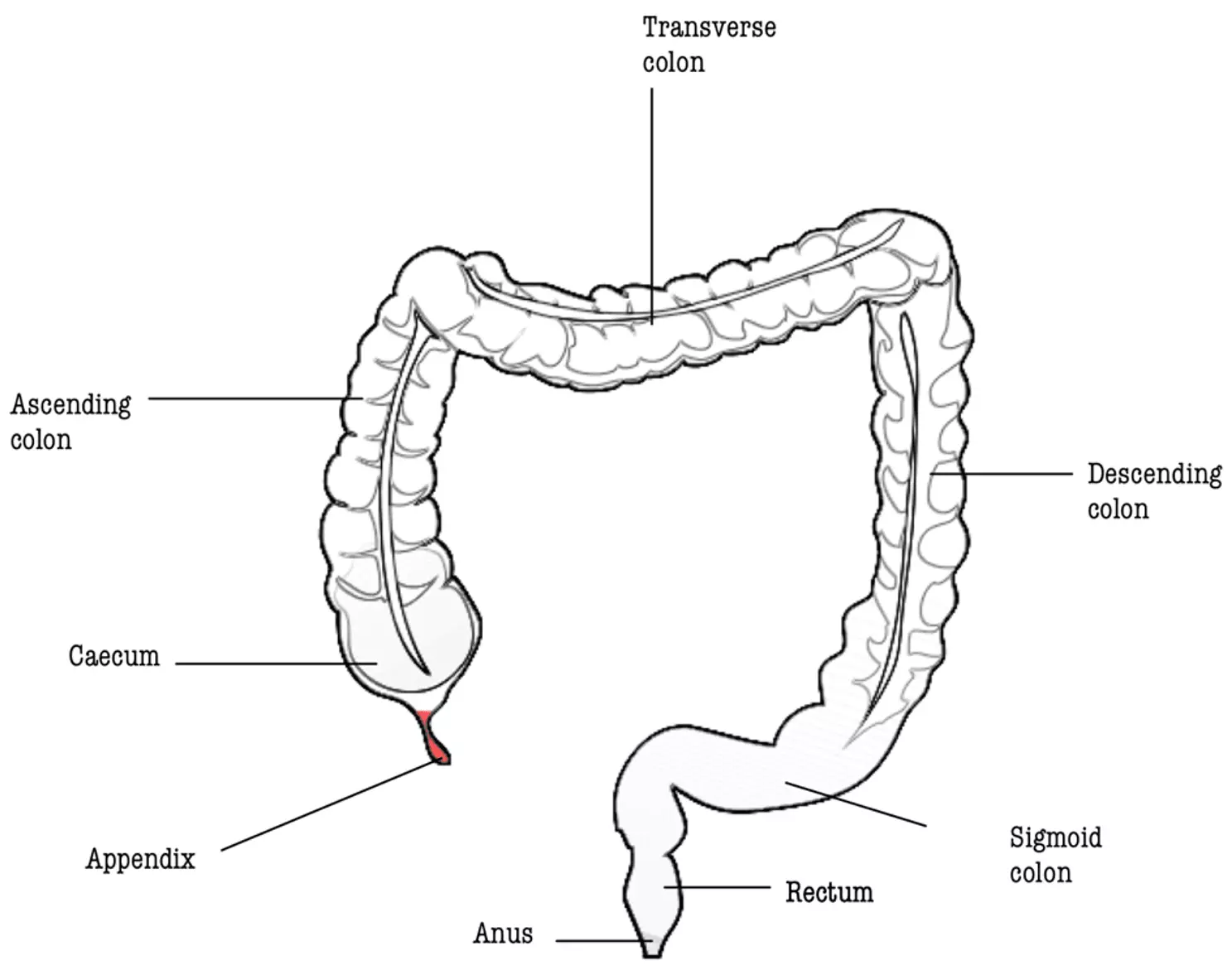
Diagram - Anatomy of the large intestine, with the appendix highlighted in red
Public Domain Source by Mikael Häggström and B jonas, edited by Dr. Laura Hansell [Public domain]
The caecum, ascending colon and transverse colon are all part of the midgut, and together with the descending and sigmoid colons (hindgut structures) they make up the large intestine.
The caecum is the most proximal part of the large intestine and lies within the peritoneum. It is the site of storage for chyme that is received from the small intestine and contains the ileocaecal valve to prevent reflux of this chyme back into the ileum. The caecum’s arterial supply is from the ileocolic artery which branches off the SMA and its venous drainage is into the ileocolic vein which drains into the SMV. Lymphatic drainage is into the ileocolic lymph nodes.
The ascending colon is retroperitoneal. Its arterial supply is from the right colic artery which branches off the SMA and its venous drainage is into the SMV. Lymphatic drainage is into the superior mesenteric lymph nodes.
The transverse colon lies within the peritoneum and has its own mesentery - the transverse mesocolon. Its arterial supply is mainly from the middle colic artery which branches off the SMA, with the distal third supplied by the left colic artery from the IMA, and its venous drainage is into the middle colic vein which drains into the SMV. Lymphatic drainage is into the superior mesenteric lymph nodes.
The colon is much wider and shorter than the small intestine, and it has crypts not villi to increase its surface area. The external longitudinal muscle of the colon is incomplete, it is made up of teniae coli (bands of muscle) which cause the formation of haustra (sacculations) when they contract.
The main functions of the colon are final water and electrolyte absorption (facilitated by ENaC channels), and the formation and temporary storage of faeces prior to defaecation.
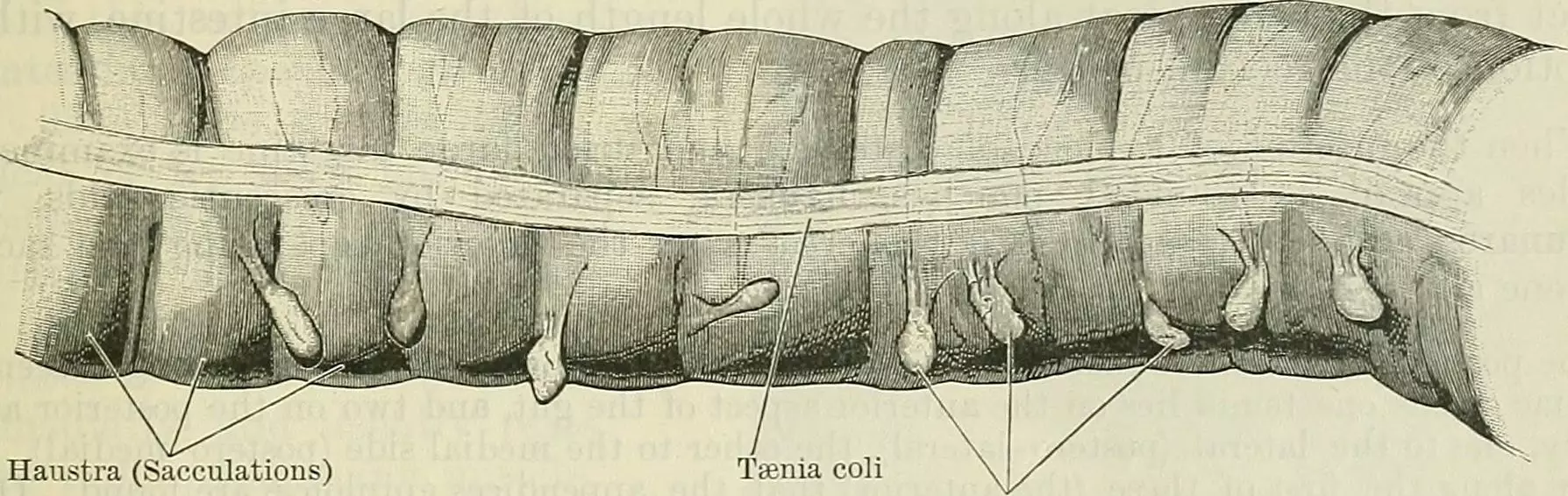
Diagram - The teniae coli and haustra of the large intestine
Public Domain Source by Cunningham's Textbook of Anatomy [Public domain]
Plain abdominal x-rays are an investigation that is rarely ordered because they cannot provide very much information about the soft tissue structures that make up most of the abdominal cavity. One of the few indications for a plain abdominal x-ray is obstruction of the bowel. In the case of obstruction, the speed of abdominal x-ray is very helpful, and being able to identify whether the obstruction is in the small or large bowel is very helpful.
There are a number of features that can help differentiate between the small and large intestine on plain film x-ray:
- The small bowel is narrower than the large bowel - the diameter of the small bowel should not exceed 3cm, whereas the large bowel can have a diameter of 6cm, or even 9cm in the caecum.
- The small bowel is often more central in the abdominal cavity, with the large bowel peripherally around the abdomen. This may be less reliable with very dilated bowel loops as can be seen in obstructions (the main indication for plain film abdominal x-rays).
- The plicae circularis traverse the whole diameter of the small bowel, whereas the haustra in the large bowel do not traverse the whole diameter.
While the interpretation of abdominal x-rays is outside the scope of this article, it is important to understand the clinical applications for the anatomical knowledge explained in this article.
Edited by: Dr. Maddie Swannack
Reviewed by: Dr. Thomas Burnell
- 5537

