Next Lesson - Chemical Control of Breathing and Plasma pH
Abstract
- Carbon dioxide is more soluble than oxygen and there is 21.1 mmol/L of carbon dioxide in arterial blood compared to 8.8 mmol/L of oxygen.
- Carbon dioxide reacts with water molecules to produce hydrogen and hydrogen bicarbonate ions.
- The pH of the plasma depends on the concentration of dissolved carbon dioxide, which depends on the partial pressure of carbon dioxide in the blood.
- There is a high concentration of hydrogen carbonate ions in the plasma. This means the majority of the dissolved carbon dioxide is prevented from reacting with the water molecules in the plasma, resulting in the pH of the plasma being alkaline (pH 7.35 - 7.45).
- The reaction between carbon dioxide and water is sped up by carbonic anhydrase in erythrocytes. The hydrogen ions react with haemoglobin, whilst the hydrogen carbonate ions move into the plasma of the blood.
- Hydrogen bicarbonate ions are able to react with acids that the body has produced (like lactic acid) and the carbon dioxide produced is breathed out resulting minimal changes to the pH of the plasma.
- There are three forms in which carbon dioxide can be transported around the body: dissolved in the plasma, in the form of hydrogen carbonate ions and carbamino compounds.
Core
In the plasma, carbon dioxide is more soluble than oxygen, meaning that there is 21.1 mmol/L of carbon dioxide in arterial blood compared to 8.8 mmol/L of oxygen. The carbon dioxide in the blood reacts with the water and haemoglobin molecules to allow this large amount of carbon dioxide to be carried. It is important to know that carbon dioxide binds to a different site to oxygen molecules on the haemoglobin molecule.
Carbon Dioxide in Arterial Blood
It seems almost wrong that arterial blood has a relatively high concentration of carbon dioxide, and this is seen as a waste product that would only be present in venous blood. However, carbon dioxide has an important role in controlling the pH of the blood, which is necessary to prevent the denaturation of proteins in the blood.
Carbon dioxide dissolves in water and once dissolved, the carbon dioxide molecules are able to react with the water molecules to form carbonic acid (H2CO3). Carbonic acid quickly dissociates into hydrogen ions (H+) and hydrogen carbonate ions (HCO3-). The reaction described is reversible, meaning it is dependent on the concentration of reactants (carbon dioxide and water) and products (hydrogen ions and hydrogen carbonate ions).
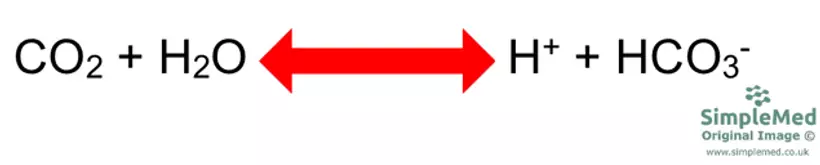
Diagram - The reaction between carbon dioxide and water to form hydrogen and hydrogen carbonate ions
SimpleMed original by Dr. Peter Parkinson
The overall pH of the plasma of the blood depends upon the concentration of dissolved carbon dioxide. A large amount of dissolved carbon dioxide will push the reaction to the right hand-side (meaning more H+ and HCO3- ions are produced), and a high concentration of H+ and HCO3- ions will push the reaction to the left hand-side (increasing the amount of CO2 produced).
The concentration of carbon dioxide dissolved in the plasma depends on the partial pressure of carbon dioxide of the blood (pCO2). This in turn depends on how much carbon dioxide is present in the alveoli (the partial pressure of carbon dioxide in the alveoli), which is controlled by ventilation rate.
If the pCO2 increases, the pH of the plasma will decrease and become more acidic because this pushes the reaction to the right, which produces more H+ ions. However, if the pCO2 decreases, the pH of the plasma will increase and become more alkaline, because this pushes the reaction to the left, which reduces the amount of H+ ions.
Blood plasma contains around 25 mmol/L of hydrogen carbonate ions, but this high amount cannot be produced by carbon dioxide dissociation alone. By having a high concentration of hydrogen carbonate ions in the plasma, the majority of the dissolved carbon dioxide is prevented from reacting with the water molecules in the plasma because the reaction wants to be pushed to the left so cannot dissolve any more CO2. This results in the pH of the plasma being alkaline, and is shown in the diagram below, with the high concentration of HCO3- ions shown as the large blue arrow.
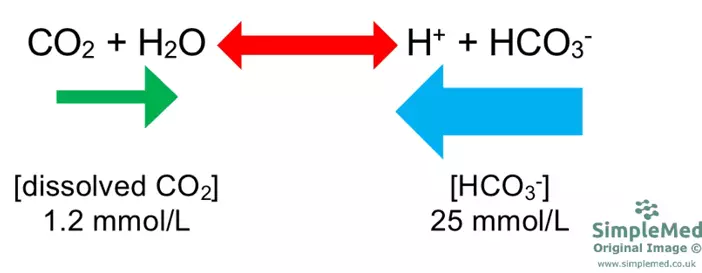
Diagram - Equation showing the high concentration of hydrogen carbonate ions preventing the dissolved carbon dioxide from reacting with the water molecules in the plasma of the blood
SimpleMed original by Dr. Peter Parkinson
It is possible to calculate the pH of the plasma by using the Henderson-Hasselbalch equation. The equation uses the values of pCO2 and concentration of HCO3- ions.
Henderson-Hasselbalch Equation: pH = pK + Log ([HCO3-] / (pCO2 x 0.03)).
The value for pK is the relative acid strength scale and is constant at 6.1 at 37oC. This means that for every pH in a human being at 37 degrees (most humans) the pK is 6.1.
The multiplication of pCO2 by 0.03 is needed because this converts pCO2 into the concentration of carbon dioxide that is dissolved in the blood (and not bound to another molecule).
It is also important to note that in this equation, HCO3- is divided by CO2. This means that if HCO3- increases, the pH will increase, but if CO2 increases, the pH will decrease. This also makes sense because CO2 dissolves to produce H+ ions.
While an understanding of this equation is important for skills like interpretation of an arterial blood gas, in clinical practice the pH is pre-recorded on the blood results.
Production and Control of Hydrogen Carbonate Ions
Within the erythrocytes, carbon dioxide reacts with water molecules within the cytoplasm of the cell to form hydrogen ions and hydrogen carbonate ions as shown above. This reaction is sped up by the action of the enzyme carbonic anhydrase.
The H+ ions then bind to the negatively-charged groups present on the haemoglobin chains, and the HCO3- ions are transported out of the cell via the chloride-bicarbonate exchanger. This means that the forward reaction is allowed to take place, because all of the H+ and HCO3- ions are removed from the cytoplasm of the cell.
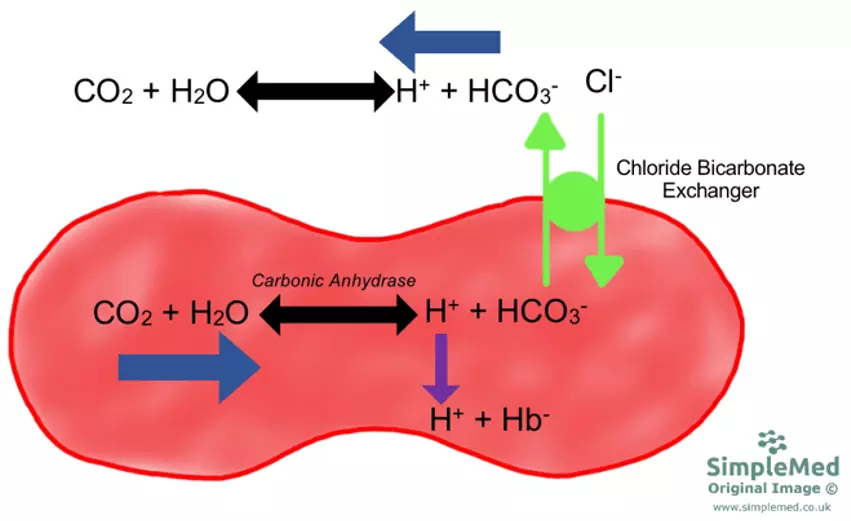
Diagram - The production of hydrogen carbonate ions in erythrocytes
SimpleMed original by Dr. Peter Parkinson
The concentration of HCO3- ions produced in this way depends on the concentration of H+ ions that bind to haemoglobin. The kidneys are responsible for controlling excretion of H+ ions in urine.
Overall, pH of the plasma depends on the pCO2 and the concentration of HCO3- ions.
Hydrogen bicarbonate ions are able to react with acids that the body produces; lactic acid from anaerobic respiration and ketones from breakdown of fatty acids. Carbon dioxide is the product of the reaction and can be removed from the body via ventilation. This results in the pH of the plasma minimally changing and HCO3- ions acting as a buffer during periods when excess acids are produced.
Eventually, the stores of bicarbonate ions in the blood can be depleted. The kidneys try to adapt to this by increasing bicarbonate reabsorption and generating new bicarbonate, but recovery from depletion can take time.
Carbon Dioxide in Venous Blood
The pCO2 is higher in the venous blood due to the tissues producing carbon dioxide during aerobic respiration. This carbon dioxide is either dissolved into the blood or bound to haemoglobin.
At the actively respiring tissues, there is a lower partial pressure of oxygen because the tissues are using it up, so the haemoglobin is in T state (meaning it is more likely to release its oxygen molecules). In this state, more H+ ions are able to bind to the haemoglobin molecule and more hydrogen carbonate ions are produced. This allows the forwards reaction to continue, because the H+ ion concentration is low, allowing more CO2 to be dissolved.
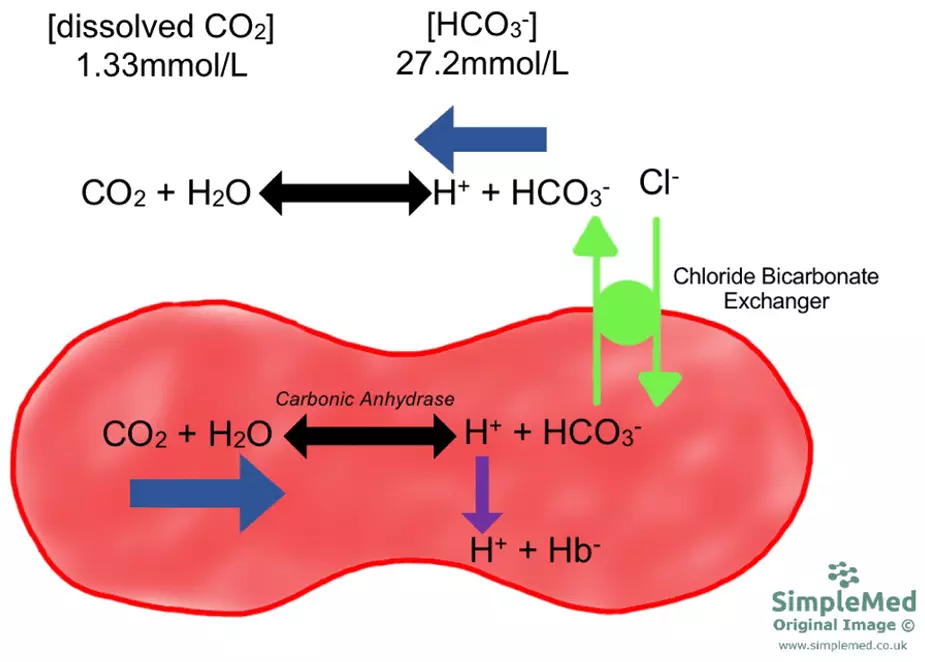
Diagram - The concentrations of hydrogen carbonate ions and dissolved carbon dioxide in venous blood
SimpleMed original by Dr. Peter Parkinson
Despite there being a higher concentration of hydrogen carbonate ions in the venous blood, the pH does not change dramatically as the pCO2 also increases (thinking back to Henderson-Hasselbalch equation).
At the lungs, the partial pressure of oxygen increases, meaning more oxygen molecules bind to haemoglobin. This causes the haemoglobin molecule to transform into its R state. This releases the bound H+ ions, which react with the HCO3- in the venous blood. This produces carbon dioxide, which is breathed out.
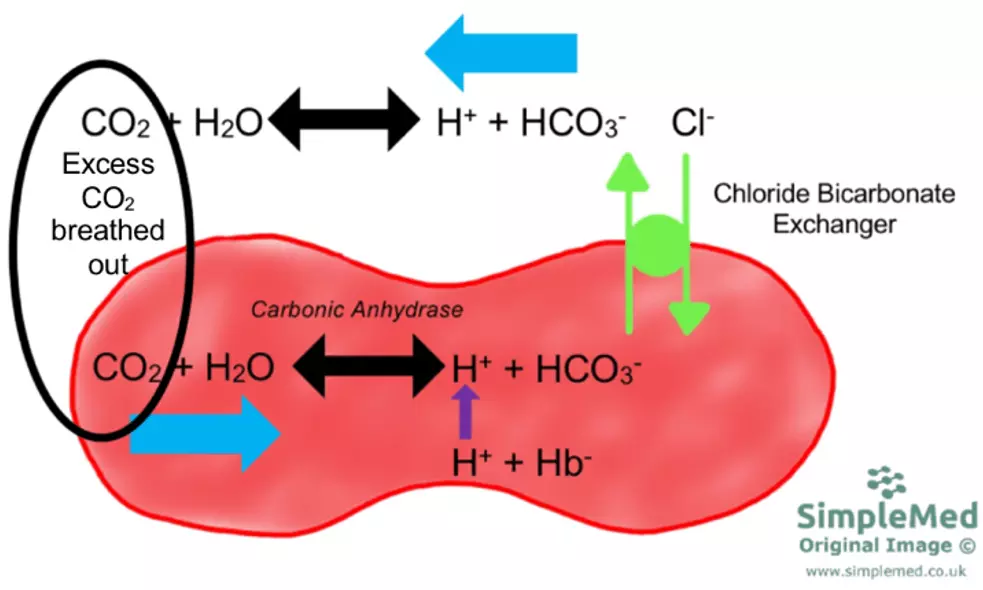
Diagram - How carbon dioxide is removed as part of carbon dioxide transport in the body
SimpleMed original by Dr. Peter Parkinson
Summary of Carbon Dioxide Transport
There are three methods of transporting carbon dioxide in the blood: hydrogen carbonate ions, carbon dioxide dissolved in the plasma, and (the one not yet explained) carbamino compounds.
Carbon dioxide can bind to the amine groups on the globin chains of haemoglobin. This form of carbon dioxide transport is called carbamino compounds and they do not take part in the acid base balance of the plasma. It is only a small amount of carbon dioxide that is transported in this way.
Overall, the majority of carbon dioxide is transported in the form of hydrogen carbonate ions, followed by carbamino compounds, with only a small amount being dissolved in plasma (because most of this is turned into bicarbonate).
Edited by: Dr. Maddie Swannack
Reviewed by: Dr. Thomas Burnell
- 9062

