By Dr. Thomas Burnell and Dr. Bethany Turner
Next Lesson - Pulses and Pressures
Abstract
- There are seven stages of the cardiac cycle, split into systole and diastole.
- The conduction system consists of the SA node, the AV node, the Bundle of His and the Purkinje fibres.
- The cardiac cycle can be used to explain the different heart sounds heard (closing of valves) and the changes seen in an ECG.
Core
The heart is an amazing pump, being able to pump 5 litres per minute, 7000 litres per day. The stages of pumping are split into diastole and systole.
Systole is when the ventricles of the heart contract to pump blood into the pulmonary or systemic circulation.
Diastole is when the ventricles relax and fill with blood.
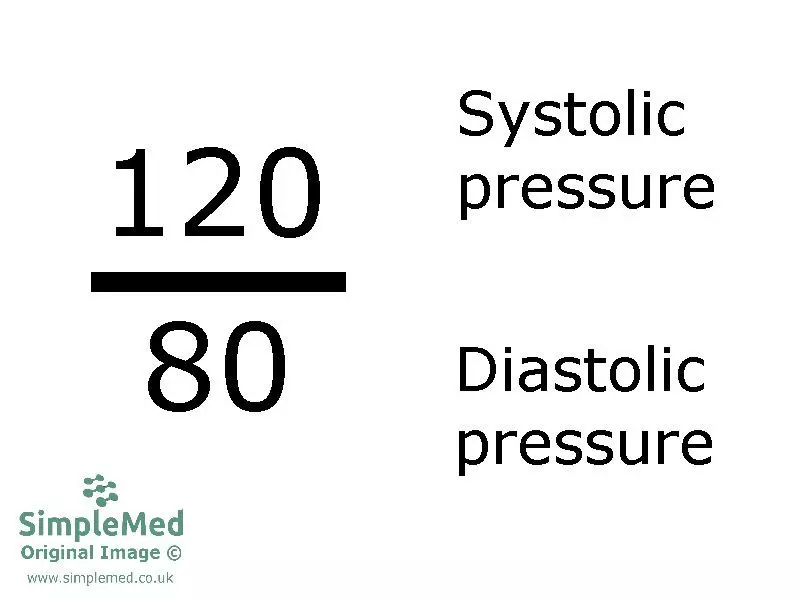
Image - The way blood pressure is shown in clinical practice. The top number is the pressure within the vessels during systole. The bottom number is the pressure within the vessels during diastole
SimpleMed original by Dr. Marcus Judge
There is a conduction system in the heart that sends electrical impulses across the myocardium (muscular tissue of the heart) to control the contraction of the atria and ventricles. The steps of the system are:
1. Pacemaker cells located within the sinoatrial (SA) node in the wall of the right atrium spontaneously depolarise, generating an electrical impulse which spreads across the atria and causes them to contract.
2. There is a fibrous band of tissue that separates the atria from the ventricles. This prevents the impulse from spreading directly to the ventricles.
3. Instead, the impulse reaches the atrioventricular (AV) node which is located between the atria and is the only physiological path through the fibrous band.
4. The AV node delays the pulse for a short period before transmitting the impulse down the bundle of His (specialised conduction fibres).
5. Once reaching the end of the bundle of His, the impulse continues to spread through the ventricle walls via the Purkinje fibres.
6. The impulse then spreads up the walls of the ventricles and causes them to contract.
This system allows the ventricles to contract in a coordinated fashion from the apex upwards towards the base of the heart to maximise the amount of blood ejected - similar to squeezing a tube of toothpaste from the bottom rather than the middle.
The regulation of the cardiac cycle and the mechanism of the action potentials is discussed in detail in the article on Cardiac Conduction.
The Wiggers diagram is used to illustrate the cardiac cycle. It shows the pressure and volume changes within the heart chambers as well as the corresponding changes on an Electrocardiogram (ECG). The diagram uses the pressure and volume changes from the left side of the heart. The right hand side shows similar changes, but as the right side operates at lower pressures they are not as pronounced. Therefore, for the purposes of illustration, the left side is used.
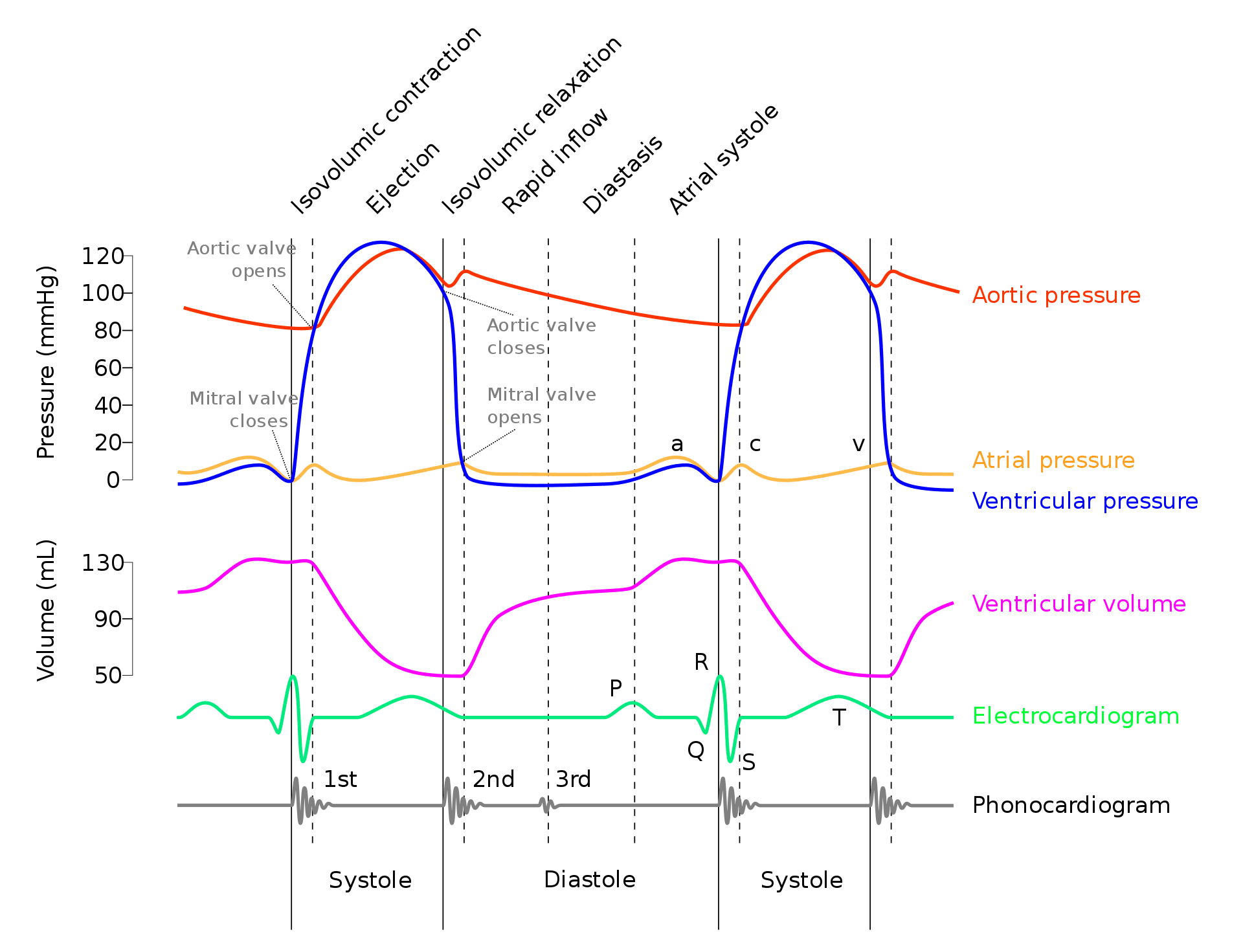
Diagram - Wiggers diagram. This shows the cardiac cycle, including the various pressures and volumes around the heart, an ECG trace (showing the electrical activity of the heart) and a phonocardiogram (showing the heart sounds - each sound corresponds to a valve shutting). It is excellent for understanding what happens in each section of the heart during the cardiac cycle. Go through it step-by-step, starting from step 1 of the cardiac cycle below, to improve your understanding
Creative commons source by adh30 revised work by DanielChangMD who revised original work of DestinyQx; Redrawn as SVG by xavax [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The cardiac cycle is split into 7 phases:
1. Atrial contraction
2. Isovolumetric contraction
3. Rapid ejection
4. Reduced ejection
5. Isovolumetric relaxation
6. Rapid filling
7. Reduced filling
Phases 2-4 are systole, and phases 5-1 are diastole.
At 67 bpm systole lasts for around 0.35 seconds and diastole for around 0.55 seconds, totalling 0.9 seconds for one cycle. Systole is relatively constant in duration compared with diastole, and at higher heart rates the reduction in cycle length occurs mainly due to shortening of diastole.
1. In atrial contraction the cells in the SA node fire an impulse which can be seen as the P wave on an ECG. This causes the atria to contract. The resulting increase in atrial pressure is seen as the ‘a wave’ on the Wiggers diagram. At the end of the previous cycle the ventricle is 90% full, with atrial contraction accounting for the final 10% of ventricular filling. End diastolic volume is now reached.
2. The next phase is isovolumetric contraction where the ventricle contracts. The QRS complex signals ventricular depolarisation. As the ventricle contracts, ventricular pressure rises above atrial, shutting the mitral valve. This can be heard as the 1st heart sound S1. When aortic and mitral valves are closed, blood cannot exit the ventricle and therefore the volume of blood in the ventricle does not change (hence isovolumetric). Bulging of the closed mitral valve into the atrium during early ventricular contraction contributes to the ‘c wave’.
3 + 4. The ejection phase is split into rapid and reduced ejection:
- In rapid ejection, ventricular pressure rises above aortic due to ventricular contraction. This opens the aortic valve and blood is forced out causing a fall in ventricular volume. There is a corresponding fall in atrial pressure seen as the X descent on the Wiggers diagram because the blood leaving the ventricle pulls on the mitral valve.
- In reduced ejection the ventricle repolarises which is seen as the T wave on an ECG. The ventricle begins to relax meaning the rate of ejection falls but as the pressure in the ventricle is still higher than the aorta, blood continues to leave. At the same time, venous blood is returning to the atrium, seen as the V wave on Wiggers diagram.
5. When ventricular pressure falls below the aortic pressure, the aortic valve closes, and isovolumetric relaxation begins. This marks the start of diastole. This closure is heard as the 2nd heart sound S2, and causes the dicrotic notch in aortic pressure. There is a rapid decline in ventricular pressure as the ventricle relaxes. The volume of blood in the ventricle does not change as no valves are open (hence isovolumetric). End systolic volume is achieved.
6. Rapid filling occurs next as atrial pressure becomes greater than ventricular, causing the mitral valve to open. Blood then flows passively into the ventricle from the atrium. The Y descent is seen in the Wiggers diagram as blood exits the atrium. Ventricular filling is normally silent, however, sometimes a 3rd heart sound S3 can be heard. This is normal in children but can be a sign of pathology in adults.
7. Finally there is reduced filling where the rate of filling slows down as the ventricle fills to about 90% of its maximum capacity. The cycle then starts again.
At the end of diastole, the volume inside the ventricles is the end diastolic volume (EDV). At the end of systole, the volume inside the ventricles is the end systolic volume (ESV). These values are important as we can use them to calculate the stroke volume (volume of blood pumped out of one ventricle).
Stroke volume = EDV - ESV.
Reviewed by: Dr. Marcus Judge
- 36444

