Next Lesson - Sepsis
Abstract
- Patients presenting with an infection need accurate diagnosis of the infective organism they are infected with to begin targeted treatment.
- To achieve this, a number of investigations can be carried out which can be used to identify the exact organism, including what drugs can be used to treat the organism.
- A gram stain is a common initial investigation used in suspected bacterial infection. It involves looking at the colour and shape of a stained bacterial sample under a microscope.
- A serology is a common investigation used to detect antigens/antibodies within the patient's blood. It can be used for diagnosing all micro-organism types.
- A PCR test can be used to detect DNA or RNA within body fluids. PCR assays are usually designed to detect specific organisms and are widely used for many bacterial and viral infections. Some PCR tests can provide results quickly, but cost and availability vary.
- A blood culture can be taken to grow any bacteria that may be present within the usually sterile blood of the patient. Whatever grows in the culture can then be tested for antibacterial susceptibility. However, this process takes a long time and is not suitable for hyper-acute situations.
- In emergency/acute situations such as sepsis or meningitis (although blood/CSF samples will be taken) treatment is usually given empirically - antibiotics against the most likely causative organism without definite diagnosis using the above techniques
Core
When a patient presents with an infection, it can often be difficult to tell the exact organism they are infected with from clinical signs and history alone. Many symptoms are common among many micro-organisms and thus investigations need to be carried out to confirm a diagnosis and begin targeted treatment.
This article covers a handful of diagnostic investigations that can be requested by a doctor to help with specific diagnosis of an infection. Some of these tests can be used for diagnosing other diseases that are not infectious in cause, but this is not within the scope of this article. Details of the methods of carrying out these investigations are not required past this level for medical students, but accurate interpretation of their results is vital.
Used for: Bacterial infections
Sample collected via: Sputum sample, stool sample, blood sample, urine sample
A gram stain involves looking at the shape and staining of a bacterial species under a microscope after carrying out a gram stain (using crystal violet and safranin).
Gram staining differentiates bacteria by the chemical and physical properties of their cell walls through detecting peptidoglycan, which is present in the cell wall of gram-positive bacteria.
To understand gram staining, an understanding of the different shapes and components of the cell walls of bacteria is required.
The gram stain is almost always the first step in the preliminary identification of a bacterial organism. While gram staining is a valuable diagnostic tool in both clinical and research settings, not all bacteria can be definitively classified by this technique.
There are 4 basic steps to performing a gram-stain:
- A primary stain of crystal violet is applied to a heat-fixed smear of a bacterial culture. Both gram-positive and gram-negative bacteria initially take up the stain.
- Iodide is added to keep the stain inside the cells and stop it from being washed out.
- Rapid decolorization with ethanol or acetone. This essentially ‘washes out’ any remaining stain from the slide or from any cells which haven’t taken up the stain.
- The gram-negative cells which haven’t taken up the initial stain will now be transparent due to the decolourization and can not be visualised. The sample is now counter-stained with safranin to visualise these cells which were not stained in the first step. Safranin is a pink colour therefore, gram-negative cells are pink in colour.
Bacterial shapes can be either:
- Coccus shaped (pl. cocci) - these bacteria look circular
- Bacillus shaped (pl. bacilli) - these bacteria look like long tubes and are sometimes referred to as “rod” bacteria
- Spirillum or spiral shaped (pl. spirilla) - seen in a small number of bacteria and a relatively uncommon finding on a gram stain
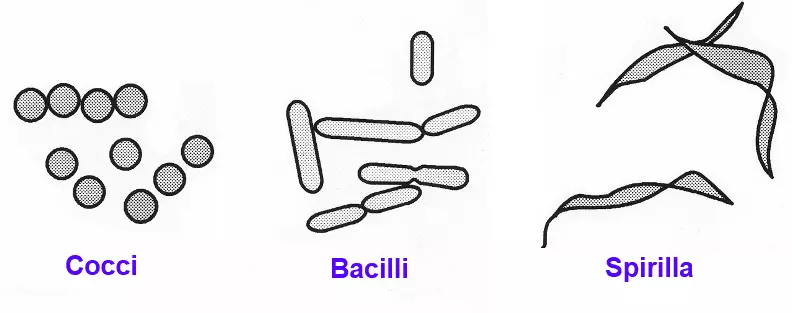
Image: The 3 shapes of bacteria. Note that cocci can arrange into singular cocci, diplococci (pairs of cocci) and larger groups such as strips and bunches
Creative commons source by CKRobinson [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The arrangement of the bacteria within space is also important. For example:
- Streptococcus species are commonly arranged in strips of cocci (memory aid: STREPS are STRIPS)
- Staphylococcus species are usually arranged in bunches (similar to grapes)
This information can be very useful in distinguishing between different species that may appear similar on a gram stain.

Figure: Gram Stain of a Streptococcus species. Notice the long chains of cocci ("strips") and purple colouring as all streptococci are gram positive. "Streps are strips!"
Public Domain Image [Public Health Image Library]
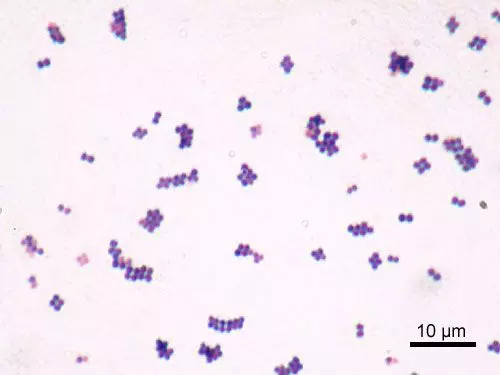
Figure: Gram Stain of a Staphylococcus species. Notice the bunches of cocci.
Creative commons source by Y Tambe [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/)]
Bacterial Cell Wall Components
Bacterial cell wall components often define how they infect the host, as well as their virulence and potential to cause disease. The cell wall components are also key in how an organism gram stains.
There are two main categories of bacteria:
- Gram-positive
- Gram-negative
Bacterial cell wall compositions vary based upon the category of bacteria:
- Gram-positive cell walls contain a plasma membrane and a LARGE peptidoglycan cell layer
- Gram-negative cell walls contain a plasma membrane a SMALL amount of peptidoglycan and then are often further encapsulated in a lipopolysaccharide cell wall (LPS) - this is a virulence factor that often leads to gram negative infections being more severe.
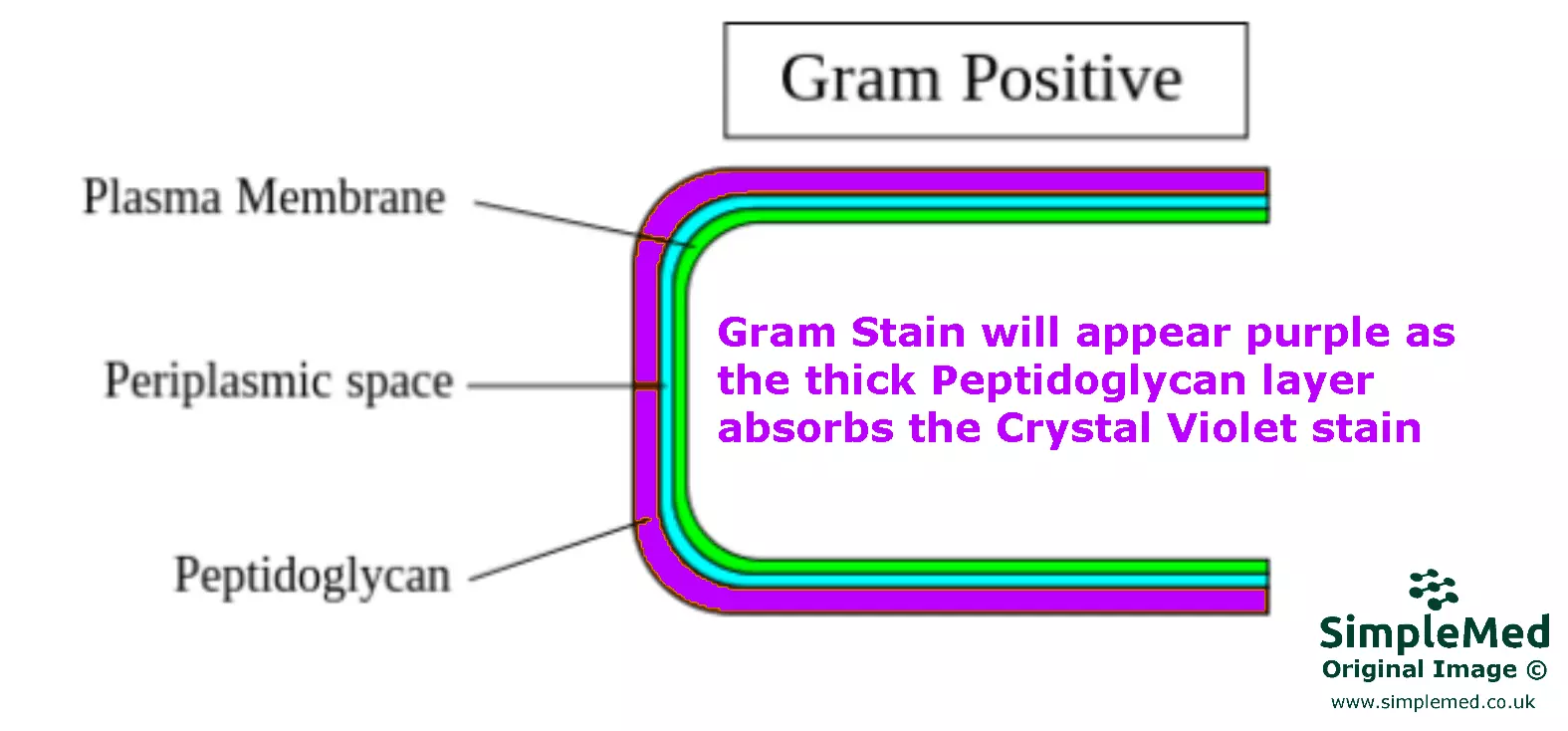
Diagram: A Gram-positive bacterial cell wall with its main components
SimpleMed original by Dr. Marcus Judge
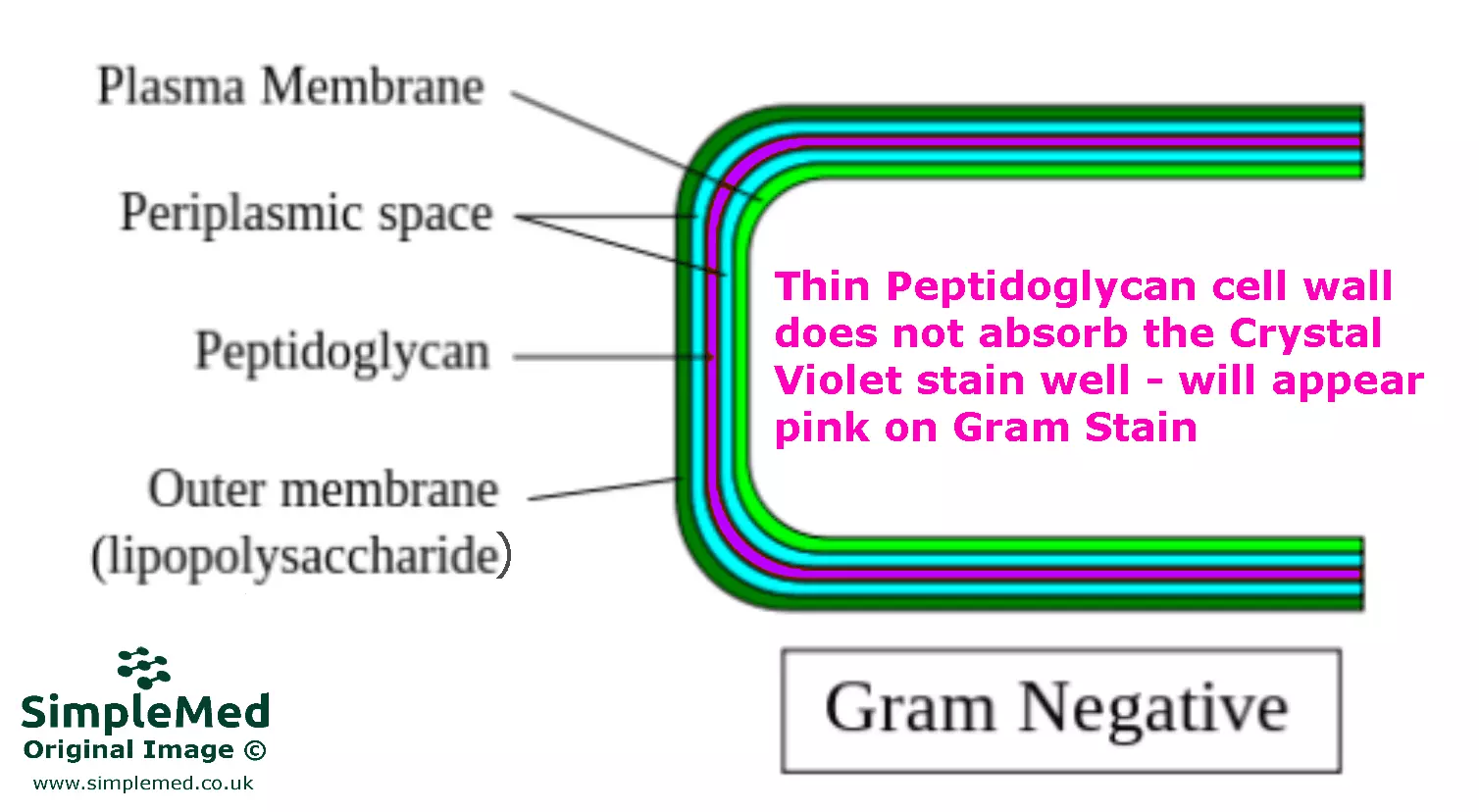
Diagram: A Gram-negative bacterial cell wall with its main components. Note the LPS outer capsule that causes serious disease and is a virulence factor
SimpleMed original by Dr. Marcus Judge
To reiterate; interpretation is carried out by analysing the colour and shape of the bacteria on the microscope slide.
Colour -
Peptidoglycan absorbs the crystal violet stain used in gram stains. As such:
- A gram-positive bacterium is PURPLE/VIOLET on a gram stain as it has more peptidoglycan.
- A gram-negative bacterium is PINK on a gram stain.
Shape -
As previously discussed, the shape of a bacterium can be either cocci, bacillus or spiral.
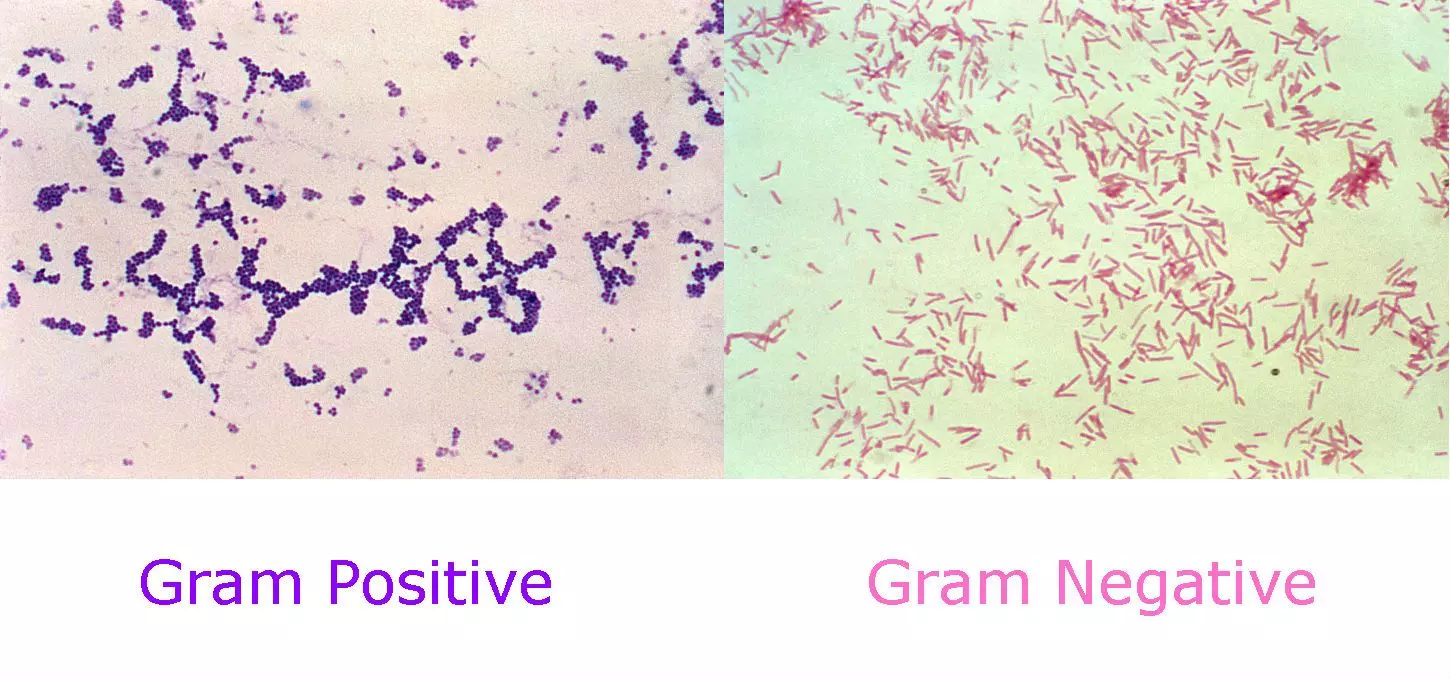
Figure: Gram Positive vs Gram Negative gram stain
Created by Dr. Marcus Judge for SimpleMed using Public Domain resources from: https://pixnio.com/science/microscopy-images/staphylococcus-aureus/photomicrograph-of-spherical-cocci-gram-positive-staphylococcus-aureus-bacteria-magnified-250x# and http://www.publicdomainfiles.com/show_file.php?id=13513615212956
Converting this information into a diagnosis
Upon knowing the colour and shape of a bacterium the current differentials can be supported or rejected. This is why knowledge of the shape and gram of common species of bacterium is important for a physician.
Here are some useful examples:
Gram positive cocci - (Purple circles)
- Staphylococcus species e.g. Staphylococcus aureus (causes cellulitis and skin abscesses)
- Streptococcus species e.g. Streptococcus pneumoniae (causes URT infections and pneumonia, is usually a diplococcus i.e. in pairs)
Often treated with: Penicillins and Carbapenems
Gram positive bacilli - (Purple rods)
- Clostridium difficile (also referred to as C.diff)(a hospital acquired infection that causes diarrhoea and other digestive complications, notable for its antibiotic resistance and spore forming ability making it hard to eradicate)
- Bacillus anthracis (commonly known as anthrax, this is a notifiable disease i.e. it must be reported to public health England if suspected)
- Listeria monocytogenes (causes listeriosis which can be an extremely severe life threatening condition)
Often treated with: Penicillins, Carbapenems and Erythromycin (macrolides)
Gram negative cocci - (pink circles)
- Neisseria meningitidis (causes meningococcal meningitis)
- Neisseria gonorrhoeae (causes gonorrhoea)
Often treated with: Cephalosporins (for example ceftriaxone, according to current UK guidance)
Gram-negative bacilli - (pink rods)
- Escherichia coli (causes gastroenteritis)
- Salmonella typhi (causes typhoid fever)
Often treated with: Cephalosporins and fluoroquinolones
Other Investigative Techniques:
Definition: Serology refers to the study of serum (blood plasma without clotting factors) but in this context is used specifically to refer to diagnostic techniques within this field of study.
Used for: All types of infections and other non-infective conditions e.g. rheumatological conditions.
Used to detect: Exposure to or infection with organisms such as Treponema pallidum (syphilis), hepatitis viruses and HIV
Sample collected via: Blood (usually), other bodily fluids
Serological tests rely on the formation of antibodies in response to an infection (against a given microorganism). Presence of these antibodies in the blood implies that the body has begun to mount an immune response (which may be ineffective) against the organism. This diagnostic test is not suitable in immunocompromised individuals as they may lack the ability to form antibodies.
There are several serology techniques that can be used depending on the antibodies being studied. These include: ELISA, agglutination, precipitation, complement-fixation, fluorescent antibodies and chemiluminescence to name but a few examples (detailed knowledge of these tests is not required for this topic).
These techniques often involve the use of complementary antibodies to detect disease marker antibodies taken from the patient’s serum. The complementary antibodies may have a fluorescent marker or cause an observable enzymatic reaction in response to signal a positive test.
Definition: A very common test carried out on the patient’s blood to detect the levels and characteristics of certain benchmark cells within the blood. Anomalies in the number of red blood cells, their size and the number of immune cells/inflammatory markers etc. can be indicative of a disease. This investigation is not inherently diagnostic but can often show if a patient is infected and what cells are being affected within the blood.
Used for: All types of infections
Used to detect:
- Sepsis (raised inflammatory markers and either extremely high or low neutrophil count depending on stage of progression)
- Advanced HIV infection may be suspected alongside other tests, but diagnosis requires CD4 T-cell measurement rather than a standard full blood count
- Epstein Barr Virus (EBV) (high lymphocytes early on in infection, low B-cell count late)
- Any other acute viral or bacterial infections (raised inflammatory markers)
Sample collected via: Blood
A full blood count is almost always requested when a patient comes in acutely ill. It provides information such as:
- White cell count
- Neutrophil count: Raised levels may indicate bacterial infection. They may also be raised in acute viral infections.
- Lymphocyte count: Higher with some viral infections such as Epstein-Barr virus (although B-cell count will drop later on in this disease’s progression when it begins to infect B-cells). Counts may be decreased by HIV infection, as this causes the destruction of T-cells.
- Raised Monocytes: May be raised in bacterial infection, tuberculosis and malaria.
- Eosinophils: Increased in parasitic infections.
- Red cell count - may be reduced in malaria and other parasitic infections that infect red blood cells and can cause anaemia.
- Platelet count - a reduced platelet count (thrombocytopenia) can be seen in severe sepsis.
See our dedicated article in the haematology section
Definition: Polymerase chain reaction (PCR) is a technique that is used to amplify trace amounts of DNA (and in some instances, RNA) located in or on almost any liquid or surface where DNA strands may be deposited. Thus, a sample of fluid or blood taken from an infected patient can be passed through a PCR machine to amplify the specific DNA/RNA strands of certain viruses/bacteria that the technician is looking for. The amplified genetic information can then be used to match the sample with a microorganism on record.
Used for: Many viral and bacterial infections where detection of specific DNA or RNA is required
Used to detect: Everything
Sample collected via: Blood, faecal sample, urine sample, throat swab, sputum sample
A PCR test is a highly sensitive and specific form of investigation commonly used in modern diagnostics, as it can detect the exact DNA of a certain microorganism within a sample and can be automated (reducing human error). It can even detect specific mutations that could cause resistance to certain medications. This allows further personalisation of treatment strategy to increase treatment efficacy.
PCR tests are powerful tools; however, they take considerable time to carry out and are far more expensive to run than a gram stain or basic serology. They can however, be used in viral infections to detect the specific infective organism.
Definition: As the name implies this technique is simply culturing a blood sample (the growing any bacteria found within the blood on a plate). It is used to detect infections have haematogenous spread (through the blood stream). This is possible as the bloodstream is usually a sterile environment; therefore any positive culture indicates pathology. The technique can be used to grow large enough amounts of the bacteria from within a patient’s bloodstream to carry out tests such as antibiotic susceptibility (to identify the best antibiotic to treat that strain of the bacteria).
Used for: Suspected Bacterial infections, particularly those with likely antibiotic resistance.
Used to detect: Bacteria
Sample collected via: Blood
The blood sample is inoculated into blood culture bottles containing nutrient broth, which provides an environment for bacterial growth. If growth is detected, organisms are then subcultured onto agar media for identification. MIC (minimum inhibitory concentration) and susceptibility testing can then be carried out on the bacteria. This test is often paired with a Gram stain test, allowing for an excellent and full diagnosis of the infection present within the patient.
It is worth remembering that all these techniques do take time, therefore in acute emergency situations such as sepsis empirical treatment must be given. Therefore, it is also useful to understand the most likely causative bacteria for infection in specific patient groups.
Edited by: Dr. Ben Appleby
- 11238

