Next Lesson - Development of the Head and Neck
Abstract
- The facial nerve supplies motor innervation to the muscles of facial expression and supplies the special sensation in the form of taste to the anterior 2/3 of the tongue.
- The vestibulocochlear nerve supplies special sensation to the ear in the form of hearing and contributes to balance maintenance.
- The glossopharyngeal nerve supplies general sensation to the tonsils and the oropharynx, supplies special sensation to the posterior 1/3 of the tongue in the form of taste, and supplies motor innervation to the stylopharyngeus muscle of the pharynx.
- The vagus nerve supplies general sensation to the larynx and supplies motor innervation to the soft palate, the larynx and pharynx.
- The accessory nerve supplies motor innervation to the sternocleidomastoid and trapezius muscles.
- The hypoglossal nerve supplies motor innervation to most of the muscles of the tongue.
Core
For an introduction to cranial nerves, including tips for remembering their names and functions, and their anatomical location, please see the first article on Cranial Nerves I-VI found here.
Pathway and Function
This nerve is responsible for both motor and sensory function. It originates from the pons and enters the petrous part of the temporal bone via the internal acoustic meatus.
From there, it can separate into 4 branches:
- Greater Petrosal - carries parasympathetic secretomotor fibres to the lacrimal glands and to glands of the nasal cavity and palate.
- Chorda tympani - provides special sensation (taste) to the anterior 2/3 of the tongue and supplies parasympathetic innervation to the submandibular and sublingual salivary glands.
- Nerve to Stapedius - innervates the stapedius muscle, a tiny muscle which acts to dampen vibrations of the eardrum to stop loud sounds damaging the ear drum.
- Nerves to the Muscles of Facial Expression (five branches remembered by the phrase ‘to Zanzibar by motor car’):
- Temporal
- Zygomatic
- Buccal
- Mandibular
- Cervical
Pathology
Depending on which branch is affected, patients can present differently. Patients may present with a facial palsy (due to paralysis of the muscles of facial expression) or other symptoms such as hyperacusis (increased sensitivity to sound), dry eyes, and altered taste. Middle ear pathology affecting the petrous bone can involve the facial nerve.
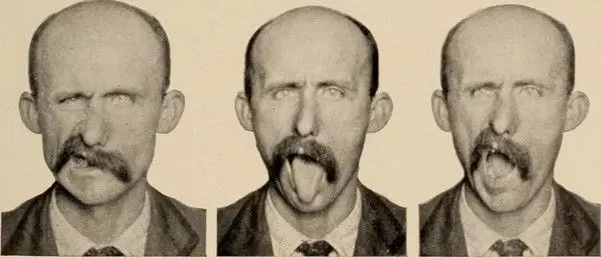
Image - Multiple pictures illustrating a facial palsy on the left side. Notice the lack of facial expression on the left
Creative commons source by Nervous and mental diseases by Church, Archibald, b. 1861 Peterson, Frederick, 1859-1938 [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Testing
Test the facial nerve by examining the muscles of facial expression - this can be done by encouraging the patient to pull faces as seen in the photograph above.
It can also be tested by eliciting the corneal reflex, as the temporal and zygomatic branches of the facial nerve supply the efferent (motor) part of this reflex.
Cranial Nerve VIII - Vestibulocochlear
Function
This nerve has two segments - the vestibular part supplying the vestibule (responsible for the special sense of balance) and the cochlear part supplying the cochlear (responsible for the special sense of hearing).
Pathway
Stemming from the inner ear, the vestibulocochlear nerve passes through the internal acoustic meatus, into the pons.
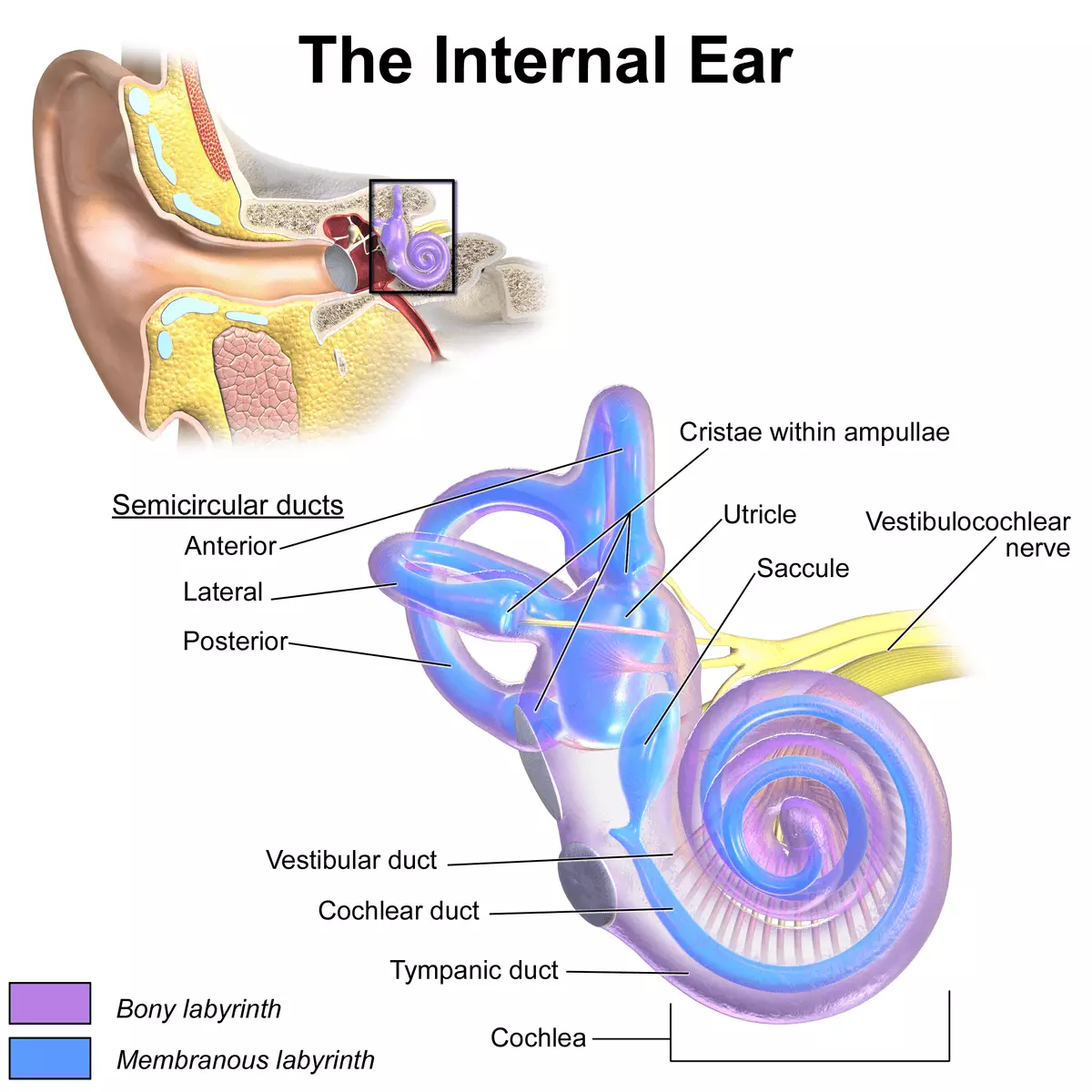
Diagram - The location of the vestibulocochlear nerve within the inner ear
Creative commons source by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436 [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Pathology
Pathology of the vestibulocochlear nerve depends on which part of the nerve is affected.
If only the cochlear portion is affected (which is rare) hearing loss will be the main symptom.
If only the vestibular portion is affected, for example by ototoxic antibiotics or Meniere’s Disease, balance issues will be the main symptom.
If both are affected together in the vestibulocochlear nerve, such as in an acoustic neuroma, hearing and balance may be affected.
Testing
Test the vestibulocochlear nerve by testing hearing (gross hearing, Weber’s and Rinne’s tests etc.), and through asking about balance.
Cranial Nerve IX - Glossopharyngeal
Function
This nerve performs multiple functions:
- Provides general sensation to the palatine tonsils, oropharynx, middle ear and tympanic membrane. It also carries sensation from the carotid body and sinus.
- Provides the sense of taste (special sensation) and general sensation to the posterior 1/3 of the tongue.
- Supplies the stylopharyngeus muscle which assists in swallowing.
Pathway
This nerve extends from the medulla and exits the skull through the jugular foramen before supplying innervation.
Pathology
Damage to this nerve can be caused by compression of the nerve by other structures for example tributaries of the carotid artery or jugular vein.
Testing
Assessment of this nerve is usually based on history and examination of swallowing and voice. The gag reflex can be elicited to demonstrate the afferent (sensory) limb, but it is often absent in healthy individuals and is not routinely required.
Function
Similar to the glossopharyngeal nerves, the vagus has multiple functions:
- Provides general sensation to the lower pharynx and larynx
- Innervates the muscles of the soft palate, pharynx and larynx to assist in speech and to elevate the soft palate.
- Provides parasympathetic innervation to thoracic and abdominal viscera.
Pathway
Originating in the medulla, the vagus nerve passes through the internal jugular foramen before running in the carotid sheath. This nerve has branches which form laryngeal nerves. The left recurrent laryngeal nerve hooks underneath the arch of aorta, whilst the right recurrent laryngeal nerve turns under the right subclavian artery.
Understanding the pathway could prove vital when considering differential diagnoses for hoarseness and dysphonia.
Pathology
Damage to this nerve can result in hoarseness of voice or dysphonia due to paralysis of the muscles of speech.
It can also lead to a deviated uvula, as the paralysed soft palate will not be able to rise, causing a deviated uvula pointing away from the pathology.
Testing
To test this nerve, examine the patient’s speech, cough and swallow. Additionally, examine for uvula deviation (when getting the patient to say ‘ahhh’). The uvula will deviate away from the side of the lesion.
The gag reflex can also be tested for this nerve, as the vagus nerve supplies the efferent (motor) arm of this reflex.
Cranial Nerve XI - Accessory Nerve
Function
Also known as the spinal accessory nerve, this nerve provides innervation to the trapezius and sternocleidomastoid (SCM) muscles.
Pathway
It has spinal roots arising from the upper cervical spinal cord, which ascend through the foramen magnum, and exits the skull via the jugular foramen before passing deep to the SCM and running posterolaterally towards the trapezius.
Pathology
Damage to this nerve can be caused by anything from stab wounds to blunt force trauma, because it has a very superficial course in the neck. It will result in paralysis of the trapezius and SCM muscles, leading to shoulder droop and difficulty abducting the arm above the horizontal.
Testing
Test this nerve by asking the patient to shrug their shoulders against resistance (trapezius) and turn their head against resistance (SCM).
Cranial Nerve XII - Hypoglossal
Function
This nerve provides innervation to all the muscles of the tongue (except the palatoglossus muscle).
Pathway
This nerve originates in the medulla and exits the skull via the hypoglossal canal. It runs just medial to the angle of mandible before innervating the muscles of the tongue.
Pathology and Testing
Test this nerve by examining the appearance and movement of the patient’s tongue. Pathology of this nerve will result in weakness and atrophy on the ipsilateral side.
This can be remembered by the phrase ‘lick the wound’ because the tongue deviates towards the injured side.
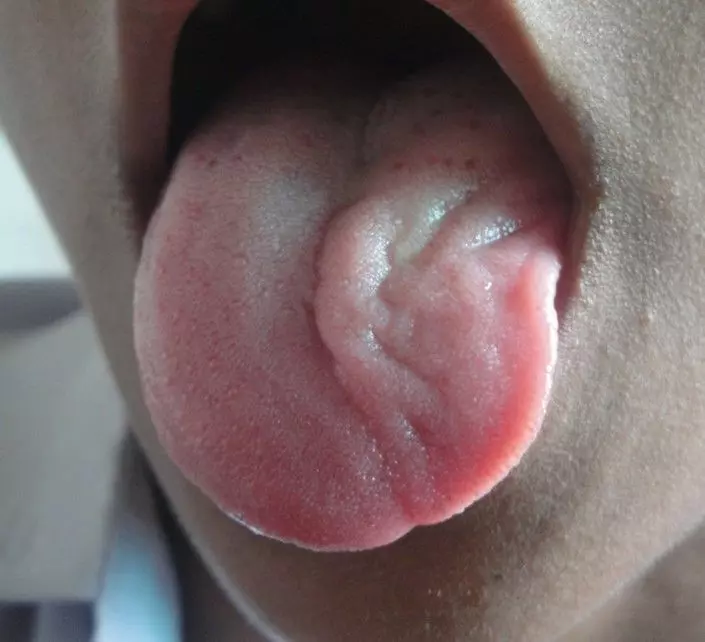
Image - Unilateral hypoglossal nerve palsy on the patient’s left side. Notice how the tongue deviates towards the left
Creative commons source by Mukherjee SK, Gowshami CB, Salam A, Kuddus R, Farazi MA, Baksh J [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Edited by: Dr. Maddie Swannack
Reviewed by: Dr. Thomas Burnell
- 8046

