Next Lesson - Fascial Planes, Muscles and Triangles
Abstract
- Ultrasound uses high frequency sound waves to produce a 2D image in real-time.
- Ultrasound is first-line for the initial investigation of neck lumps and carotid atherosclerosis.
- Radiography of the head and neck is becoming increasingly uncommon, but may be used for initial assessment of head and C-spine trauma
- CT scans use multiple X-rays to produce cross-sectional images.
- CT is first-line imaging of choice for head trauma and acute focal neurology.
- A CT window can be used to enhance the contrast between materials of similar density.
- MRI uses a magnetic field and radio waves to produce cross-sectional images.
- MRI provides the highest quality soft tissue imaging, however, it is slower and more expensive.
Core
Ultrasound uses high frequency sound waves (typically around 2 to 15 MHz) to produce a 2D image. The ultrasound transducer produces the ultrasound waves, which travel through the tissues and are reflected back to varying degrees, depending on the density of the tissue encountered. These ‘echoes’ are interpreted in terms of space and contrast in order to produce a 2D grayscale image in real-time.
Advantages of USS:
- It is cheap and widely available.
- It is very good for soft tissue imaging.
- It produces a dynamic image.
- Doppler imaging can be used to assess blood flow.
- Does not involve ionising radiation (unlike x-ray/CT).
Disadvantages of USS:
- Quality is highly user-dependent due to high level of skill required.
- Not very useful for assessing deep structures or dense tissues (e.g. bone).
Uses of USS in the head and neck:
- Imaging of the thyroid - e.g. Goitre, thyroid mass
- Evaluation of other neck lumps
- Evaluation of superficial infections - e.g. Neck abscess
- Carotid Doppler - used to assess stenosis of the carotid artery due to an atheroma
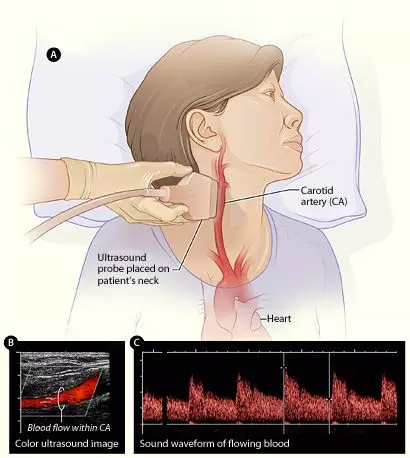
Diagram - Doppler ultrasound of the carotid artery
Creative commons source by National Heart Lung and Blood Insitute (NIH) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
A radiograph uses X-rays to produce a static 2D image. A beam of X-rays is produced and transmitted through the body. As the x-rays pass through the body, they are absorbed to varying degrees by the body’s tissues. Denser tissues (e.g. bone) absorb more x-rays while softer tissues (e.g. muscle) absorb fewer x-rays. The x-rays that remain unabsorbed reach the detector plate and turn the image dark. Therefore, dense structures appear white while less dense structures appear dark. The pattern of absorption is interpreted by a computer which produces the image.
Advantages of radiographs:
- They are cheap, quick and widely available.
- Good for assessing bone and joint pathology.
- Involves a much smaller dose of radiation compared to CT.
Disadvantages of radiographs:
- Poor soft tissue information.
- Involves a small dose of ionising radiation, therefore carrying an increased risk of carcinogenesis.
Uses in the head and neck:
- Minor head trauma (rarely used; only when CT is not indicated based on clinical decision rules)
- Cervical spine trauma
- Maxillofacial trauma
- Foreign body within neck
X-rays of the skull are becoming increasingly uncommon due to the increasing availability and superior sensitivity of CT imaging.
The cranial vault is viewed using PA (posterior-anterior) and lateral films. In normal anatomy the suture lines and blood vessels will be visible, which to the untrained eye may be mistaken for a fracture.

Image - Normal lateral radiograph of the skull. Note the visibility of the coronal suture and blood vessels
Creative commons source by Hellerhoff [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The facial skeleton is assessed with occipito-mental views (Water’s views) taken at 0 and 30 degrees angulation. A Water’s view can also be useful in assessing the paranasal sinuses.
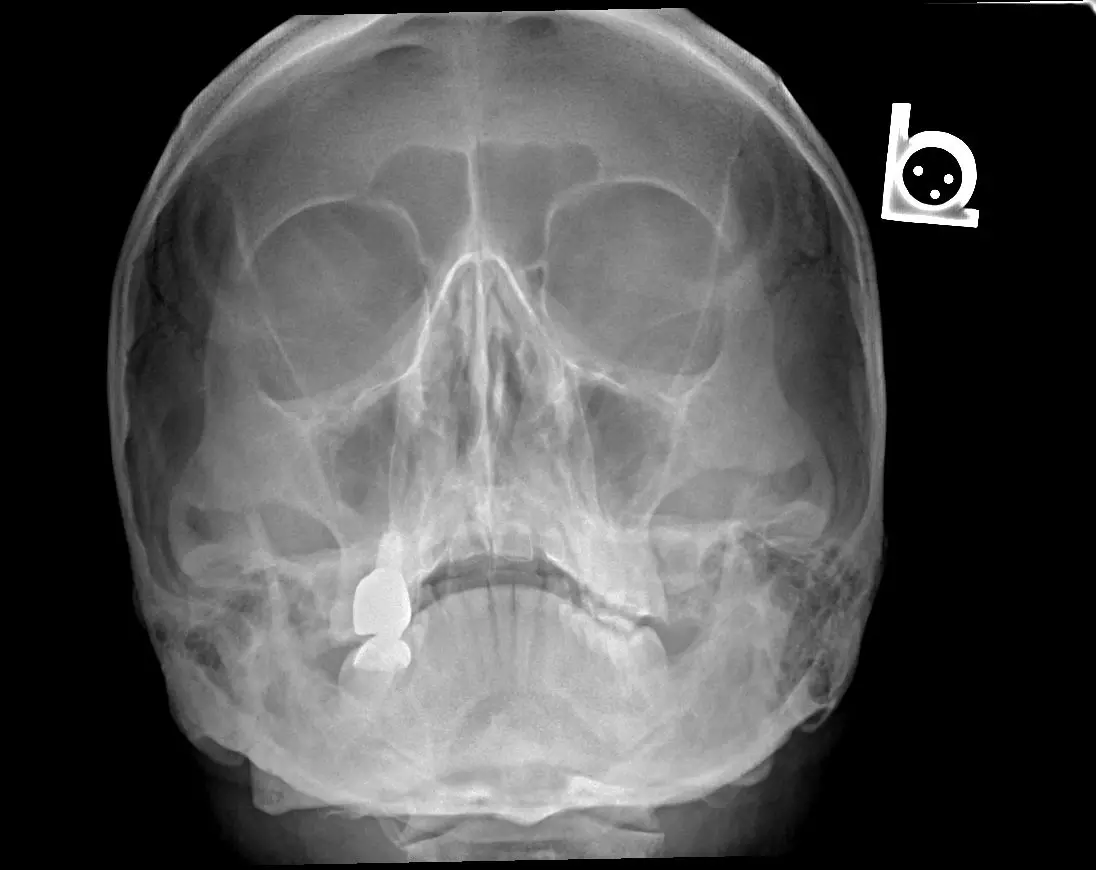
Image - Occipito-mental projection (Water’s view) of the skull
Creative commons source by Ptrump16 [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The mandible and temporomandibular joint (TMJ) are assessed with an orthopantomogram (OPG) and mandible views. The mandible commonly fractures in two places, or is accompanied by dislocation of the TMJ.
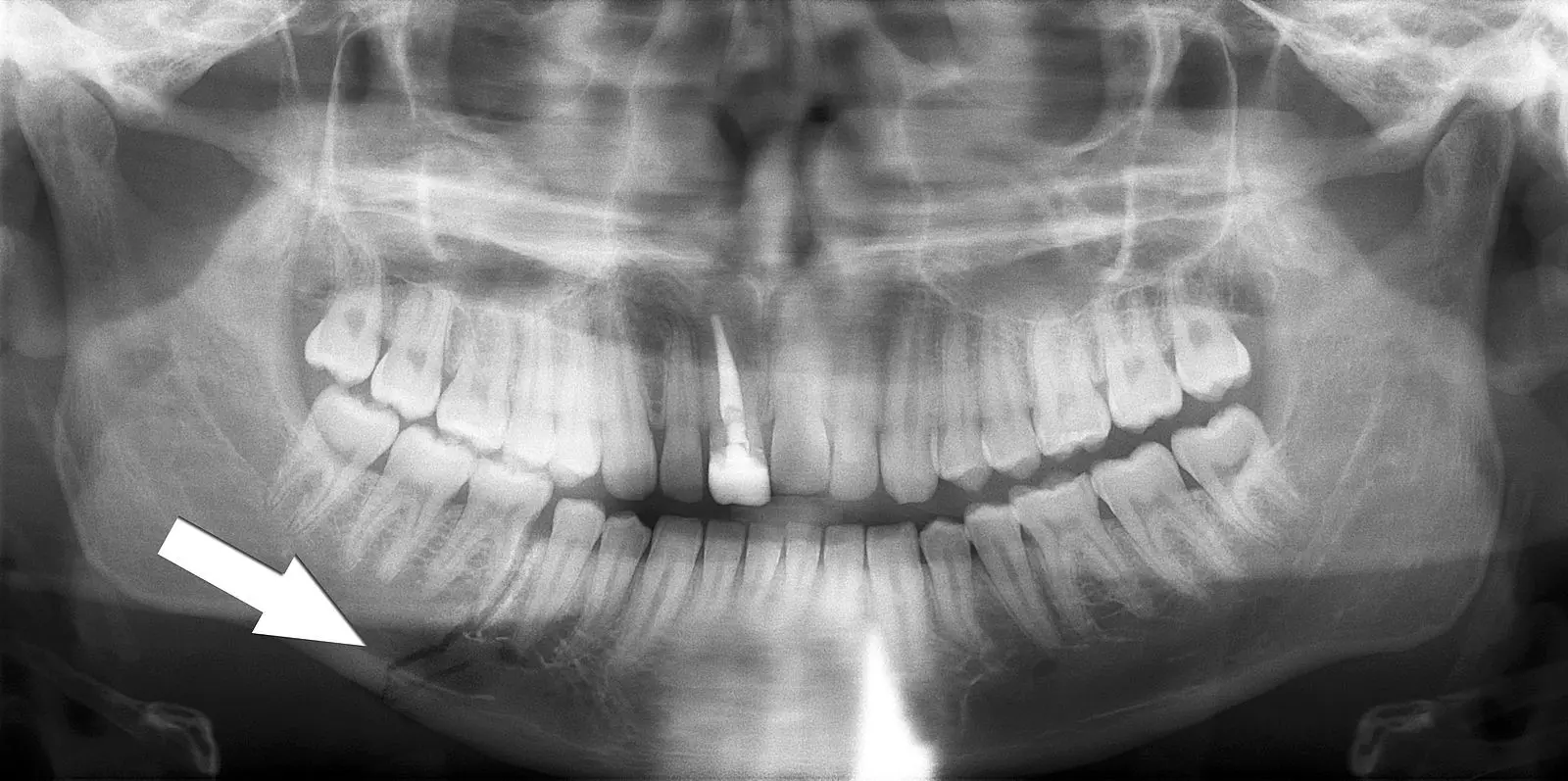
Image - Orthopantomogram showing a fracture through the body of the mandible
Creative commons source by Coronation Dental Specialty Group [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
When imaging the C-spine, AP (anterior-posterior), lateral and ‘open mouth’ views are taken. A Jefferson fracture refers to a fracture of the atlas (C1). A Hangman’s fracture refers to a fracture through the pars interarticularis of C2. A fracture of the odontoid peg is best seen with an ‘open mouth’ view. For more information, check out our article on Conditions of the Back and Neck.

Image - Lateral radiograph of the C-spine showing a Jefferson’s fracture (C1)
Creative commons source by James Heilman, MD [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
CT scans project multiple x-rays from different angles in order to produce 2D cross-sectional images which can potentially be reconstructed into a 3D image.
An important concept in CT imaging is windowing. Consider the CT scan as a greyscale image: depending on the density of the tissue, the tissues will show up as different shades of grey, with most dense structures appearing white and the least dense structures appearing black. Due to such a wide range of densities, it can be difficult to contrast tissues of similar densities as they will appear as very similar shades of grey. A CT window allows us to focus in on a certain range of densities, measured in Hounsfield Units (HU). This enhances the contrast between the structures whose density falls within this window. In essence, it allows us to better distinguish between similar shades of grey. Common CT windows that are used include bone windows, brain windows and lung windows.
Advantages of CT:
- Much better detail of bone, soft tissue and the brain compared to plain radiographs, however, the soft tissue detail is inferior to MRI.
- It is much quicker than MRI and is therefore better for acute presentations.
Disadvantages of CT:
- Involves a significant dose of ionising radiation, therefore increased risk of carcinogenesis.
- Soft tissue detail is not as high quality compared to MRI.
Uses in the head and neck:
- Head trauma - particularly to check for intracranial haemorrhage
- Maxillofacial trauma
- Cervical spine trauma
- Acute focal neurology - particularly to rule out haemorrhagic stroke
- Infection - e.g. meningitis, encephalitis (CT often initial, MRI preferred where available)
- Angiography - to evaluate the Circle of Willis and venous sinuses
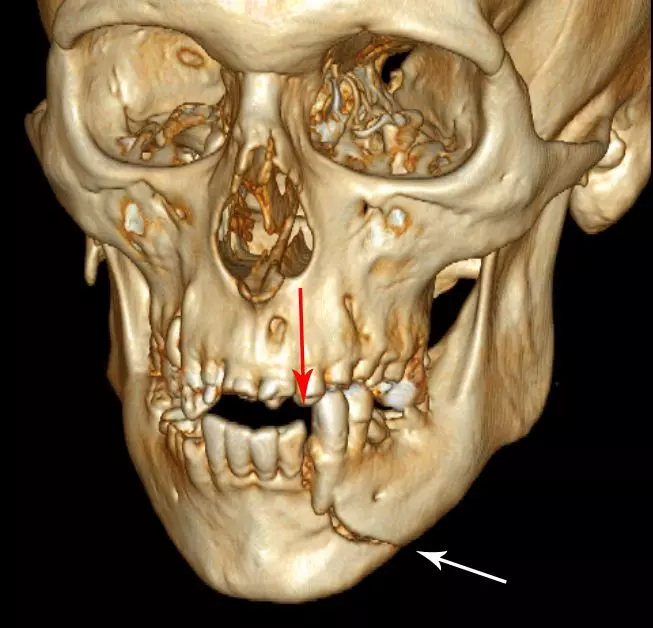
Image - 3D CT reconstruction showing a fracture through the body of the mandible
Creative commons source by Coronation Dental Specialty Group [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
CT plays an important role in the diagnosis of intracranial haemorrhage (ICH). There are 3 main types of ICH:
- Extradural - an arterial bleed (usually middle meningeal artery) secondary to head trauma. Blood collects between the periosteal dura and inner table of bone. It appears as a wedge-shaped area of hyperdensity which is bound by the suture lines.
- Subdural - bleeding from bridging veins due to trauma. Can be acute or chronic. Blood collects within the subdural space. It has a crescentic shape. Acute bleeds appear bright (hyperdense) on CT whereas chronic bleeds appear darker (hypodense).
- Subarachnoid - bleeding from one of the cerebral arteries. Can be spontaneous (ruptured berry aneurysm) or traumatic. The classical CT appearance is a central star-shaped area of hyperdensity as blood enters the subarachnoid space and collects within the basal cisterns.

Image - Axial CT head showing a spontaneous subarachnoid haemorrhage
Creative commons source by James Heilman, MD [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Magnetic Resonance Imaging (MRI)
MRI uses a strong magnetic field and radio waves to produce very detailed cross-sectional images, which can potentially be reconstructed into a 3D image.
Advantages of MRI:
- Provides very high soft tissue resolution, allowing for accurate assessment of tissue margins.
- Does not involve any ionising radiation.
Disadvantages of MRI:
- It is an expensive imaging modality.
- It usually takes longer than CT and may be less suitable in some acute presentations.
- The MRI scanner is noisy and an enclosed space, which can be distressing to some patients.
- MRI is contraindicated in the presence of certain non-MRI-compatible metallic foreign bodies due to the strong magnetic field.
Uses in the head and neck:
- Imaging of the brain, e.g. epilepsy, tumour evaluation
- Spinal cord pathology
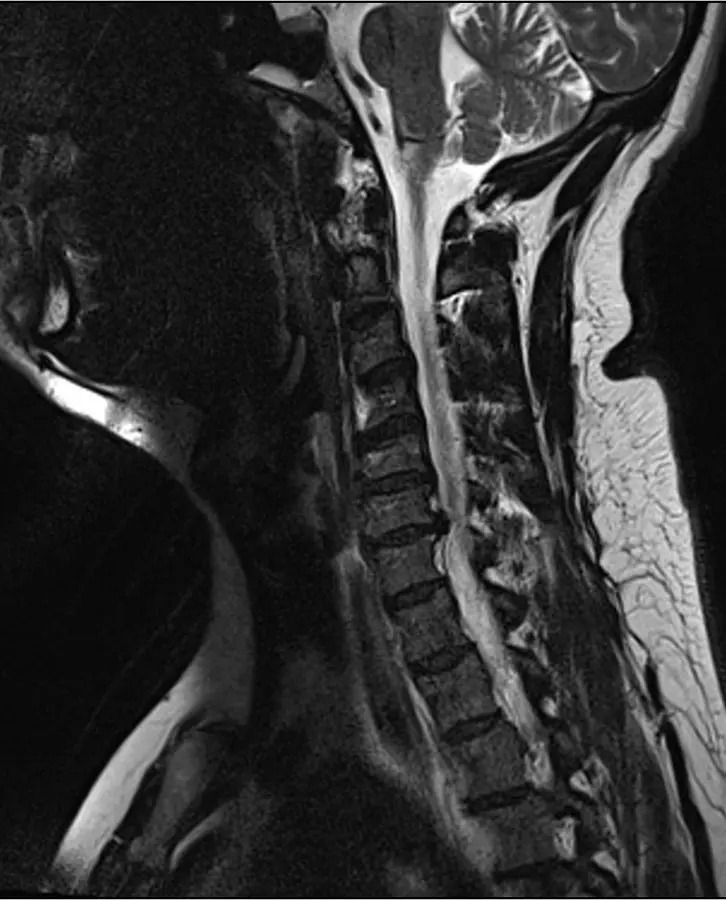
Image - Sagittal MRI of the cervical spine showing herniation of the C6/C7 intervertebral disc
Creative commons source by user:Anthonp [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Reviewed by: Dr. Thomas Burnell
- 4420

