Next Lesson - Conditions of the Back and Neck
Core
Want more information on anatomy before you begin looking at conditions? Head to our article on The Spine for more information!
Spondylosis is the term used to describe chronic degenerative changes of the spine, including degeneration of the intervertebral discs and osteoarthritis of the facet joints, most commonly affecting the lumbar or cervical spine. It is usually caused by disc degeneration and marginal osteophytosis (bony spurs developing adjacent to the end plates of the disc).
It can present with radiculopathy causing dermatome/myotome symptoms. X-ray, MRI, and CT scans can be used in diagnosis but are not definitive alone. Treatment is conservative in nature and focuses on lifestyle modifications, pain management and physiotherapy.
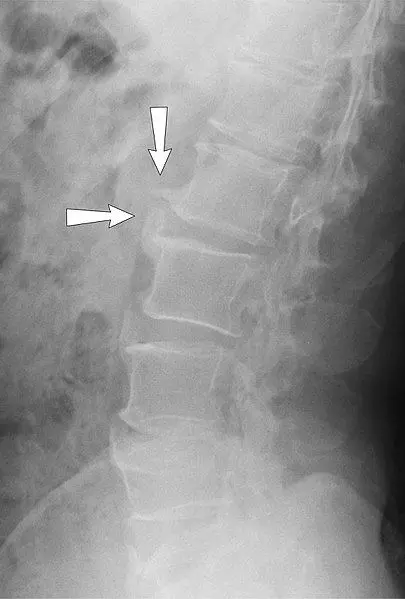
Image - An X-ray showing the lateral view of lumbar spine spondylosis
Creative commons source by Nevit Dilmen and annotated by Mikael Häggström, M.D [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Spondylolisthesis is the anterior displacement of the above vertebra on the below vertebra (commonly the 5th lumbar vertebra on the sacrum). Causes are divided into five categories: congenital/dysplastic, isthmic, degenerative, traumatic and pathological.
It can be asymptomatic, but may present with lower back pain, sciatica and/or neurogenic claudication (pain/paraesthesia in the legs when standing or walking that is relieved by rest). Diagnosis is usually confirmed with a standing X-ray, which demonstrates the vertebral displacement. Clinical examination may reveal signs of nerve root irritation if there is associated neural compression.
Treatment depends on severity, but often starts with rest, painkillers and physiotherapy. If very severe, surgery can be recommended to fuse the slipped vertebra to the adjacent vertebra using metal screws and rods.

Image - An X-ray of Spondylolisthesis
Creative commons source by Jojo [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Mechanical back pain is an extremely common condition, and the source may be in the spinal joints, the intervertebral discs, the vertebrae themselves or the surrounding soft tissues (like ligaments or muscles). It presents with back pain when the spine is loaded that worsens with activity and is relieved with rest. Risk factors for mechanical back pain include: poor posture, sedentary lifestyle, poor lifting technique and being overweight. Management involves lifestyle modifications and pain management, commonly with NSAIDs.
Sciatica is pain/paraesthesia caused by compression of the sciatic nerve or by one or more of the contributing spinal nerves (L4-S3). It presents with pain in the lower back and buttocks that radiates to one or more of the following dermatomes:
- L4: Anterior thigh and knee, and medial leg
- L5: Lateral thigh and leg, and dorsum of the foot
- S1: Posterior thigh and leg, and sole of the foot
Sciatica usually self resolves within 4-6 weeks. If symptoms are severe or persistent, the GP may suggest exercises and stretches, prescribe additional painkillers and refer to physiotherapy.
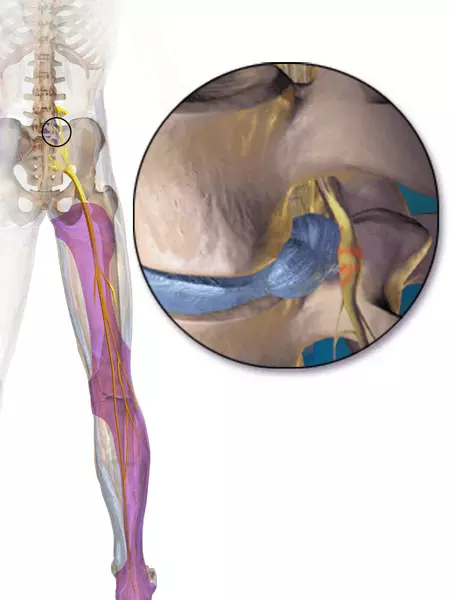
Image - The distribution of pain/paraesthesia in sciatica
Creative commons source by BruceBlaus [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Cauda equina syndrome is an absolute emergency and involves the compression of the cauda equina (a bundle of spinal nerves at the base of the spine), often due to a prolapse of a disc or a tumour that is impinging on the spinal canal . It presents with bilateral sciatica, perianal numbness, painless retention of urine, faecal incontinence and/or erectile dysfunction.
Diagnosis is confirmed by a CT or MRI scan. Urgent surgical decompression (within 48 hours of sphincter symptoms) is recommended to prevent long term neurological damage.
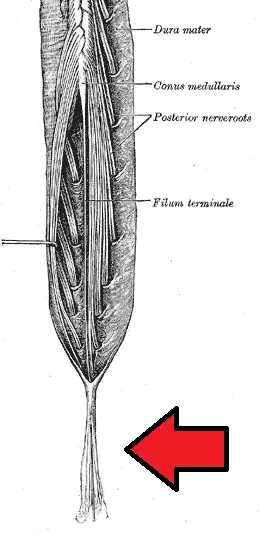
Diagram - The bundle of lumbar and sacral nerve roots that is compressed in cauda equina syndrome. The arrow points to the cauda equina
Creative commons source by Henry Gray [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Disc herniation (also known as a slipped disc) is divided into 4 stages:
- Disc degeneration- intervertebral discs dehydrate and bulge, decreasing disc height and altering load stresses on the joint.
- Disc prolapse- protrusion of the nucleus pulposus (still within the annulus fibrosis).
- Disc extrusion- nucleus pulposus exits the annulus fibrosis.
- Disc sequestration- nucleus pulposus enters the spinal canal.
It most commonly occurs at L4/5 or L5/S1 and the most common type of herniation is a para-central prolapse, meaning that the disc prolapse is off-centre (96% of cases), but can be a central prolapse (2% of cases) or a lateral prolapse (2% of cases). Disc herniation commonly presents with unilateral back pain and paraesthesia that radiates into dermatomes supplied by the affected nerve roots.
MRI provides the most conclusive evidence for diagnosis of a disc herniation, with CT used if MRI is contraindicated. Plain X-rays do not show disc herniation but may be used to assess alternative causes of back pain. Treatment is pain management, physiotherapy, weight control and surgery if the case is causing severe pain.

Image - An MRI of a L4/L5 disc herniation
Creative commons source by Edave [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Infections of the spine include: vertebral osteomyelitis (infection of the bone), discitis (infection of the disc) and epidural abscesses. They are most commonly caused by haematogenous spread (via the blood) of an infection from another location but can also be due to direct inoculation during an invasive spinal procedure (e.g. a lumbar puncture) or via spread from adjacent soft tissues. They can present with neurological damage as well as systemic symptoms such as pyrexia.
Treatment includes IV antibiotics and in severe cases surgical intervention may be required.
Reviewed by: Dr. Thomas Burnell
Edited by: Dr. Maddie Swannack
- 6928

