Next Lesson - Vitamin B12 and Folate
Abstract
- Anaemia is a sign of underlying pathology, defined by a reduced red blood cell or haemoglobin count.
- There are multiple causes of anaemia, usually due to a disruption in the normal life cycle of a red blood cell (production - circulation - destruction).
- Anaemia can be classified by the appearance of red blood cells into; microcytic, normocytic and macrocytic anaemias. It can also be classified by the cause e.g. haemolytic anaemia is caused by red cell breakdown.
- The presentation of anaemia is usually due to insufficient oxygen supply in the body.
- Treatment is dependent on the underlying cause.
Core
Anaemia is defined as the condition in which your body has insufficient haemoglobin to meet its needs. Without the correct levels, the body is unable to carry enough oxygen to its cells for them to carry out their normal function.
The clinical definition of anaemia in non-pregnant adults is a haemoglobin level below 130 g/L for males and below 120 g/L for females. However, these boundaries can vary greatly depending on factors such as race and other medical conditions.
Anaemia is not a standalone diagnosis, but a sign of underlying pathology.
Anaemia can take place due to a variety of disruptions to the life cycle of a RBC. The lifecycle of a RBC is split into 3 stages:

Diagram: Shows the lifecycle of a red blood cell and where they are found during each stage
SimpleMed original by Dr. Keertana Anne
Abnormalities during production:
Dyserythropoiesis
This is the development of defective RBCs. It can be congenital, inherited or acquired. Examples of congenital or inherited include congenital dyserythropoietic anaemia (CDA).
Acquired dyserythropoiesis can take place when the bone marrow is unable to produce enough RBCs. This can be due to damaged bone marrow from chemotherapy drugs or infection. Another more common cause of acquired dyserythropoiesis is chronic disease and inflammation, which in itself has a variety of causes ranging from renal disease (reduced erythropoietin production) to rheumatoid arthritis (a cause of anaemia of chronic disease which increases the uptake of iron into cells and reduces the amount available for RBC production).
[Further discussed in Iron Metabolism, Vitamin B12 and Folate]
Defects in haemoglobin synthesis
There are two major causes of defective haemoglobin to be produced. The first is a deficiency in essential substances in the body - iron, vitamin B12 and folate. Any deficiency in these leads to a lower RBC production as they are key in haemoglobin synthesis. The second cause is due to mutations in the proteins that form the globin chains of haemoglobin. These are seen in thalassaemias and sickle cell disease.
[Further discussed in Haemoglobinopathies]
Abnormalities during circulation:
Damage to red cells - Haemolytic anaemia
Haemolysis is the destruction (lysis) of RBCs. It can occur either in the blood vessels themselves (intravascular haemolysis), or in the spleen (extravascular haemolysis). RBCs are damaged due to shear stress, a form of mechanical damage to the cells. This occurs when they are forced through small gaps in vessels or valves. Examples include, damaged heart valves, vasculitis and microangiopathic haemolytic anaemia (MAHA) related to disseminated intravascular coagulopathies. The remnants of lysed cells can be seen on blood films in the form of schistocytes (see article on Full Blood Count and Blood Films).
Both heat damage and osmotic changes can also cause damage to the structure of RBCs. These all come under acquired causes of haemolytic anaemias.
There are also inherited causes of RBC damage. These include: hereditary spherocytosis (RBCs are spherical instead of having a biconcave shape due to defective cell membrane proteins, making them more fragile), glucose-6-phosphate dehydrogenase deficiency (G6PD deficiency) and pyruvate kinase deficiency (these last two are common causes of haemolytic anaemia, and cause an increased RBC breakdown). As the cells are abnormal the spleen removes them from circulation and destroys them, which is known as extravascular haemolysis.
The body can also attack its own RBCs, in a condition known as autoimmune haemolytic anaemia. Autoantibodies produced by your immune system bind to the proteins on the RBC membrane, causing the RBCs to be targeted and destroyed. This can be caused by other diseases (lupus, lymphomas, certain viruses like EBV/HIV) and some types of medications (e.g. penicillin).
Damaged RBCs are removed from circulation via the red pulp in the spleen, and when this happens repeatedly the bone marrow struggles to keep up with the body’s requirements as RBCs are often destroyed faster than they can be replaced.
Excessive bleeding
Anaemia can also develop in situations of blood loss (seen in injury, surgery or childbirth). When there is a large loss of blood, there is a reduced level of iron in the body, so the bone marrow is unable to increase the production of new cells to replace those that were lost. A common cause of this is menorrhagia, heavy blood loss during menstruation. Therefore it is imperative to take a full bleeding history when assessing a patient for anaemia.
Removal by Reticuloendothelial System (RES)
The RES removes damaged RBCs from the circulation, and this can become an issue when RBCs are destroyed faster than they can be replaced. An overactive RES speeds up the process of red cell destruction, and can be seen in hypersplenism.
Anaemia can be classified by the morphology of RBCs seen in the body, and also if there is an appropriate response by reticulocytes to the present pathology (for example, are there more RBCs being produced to counter the loss?). The following flow diagram can help to narrow down the causes:
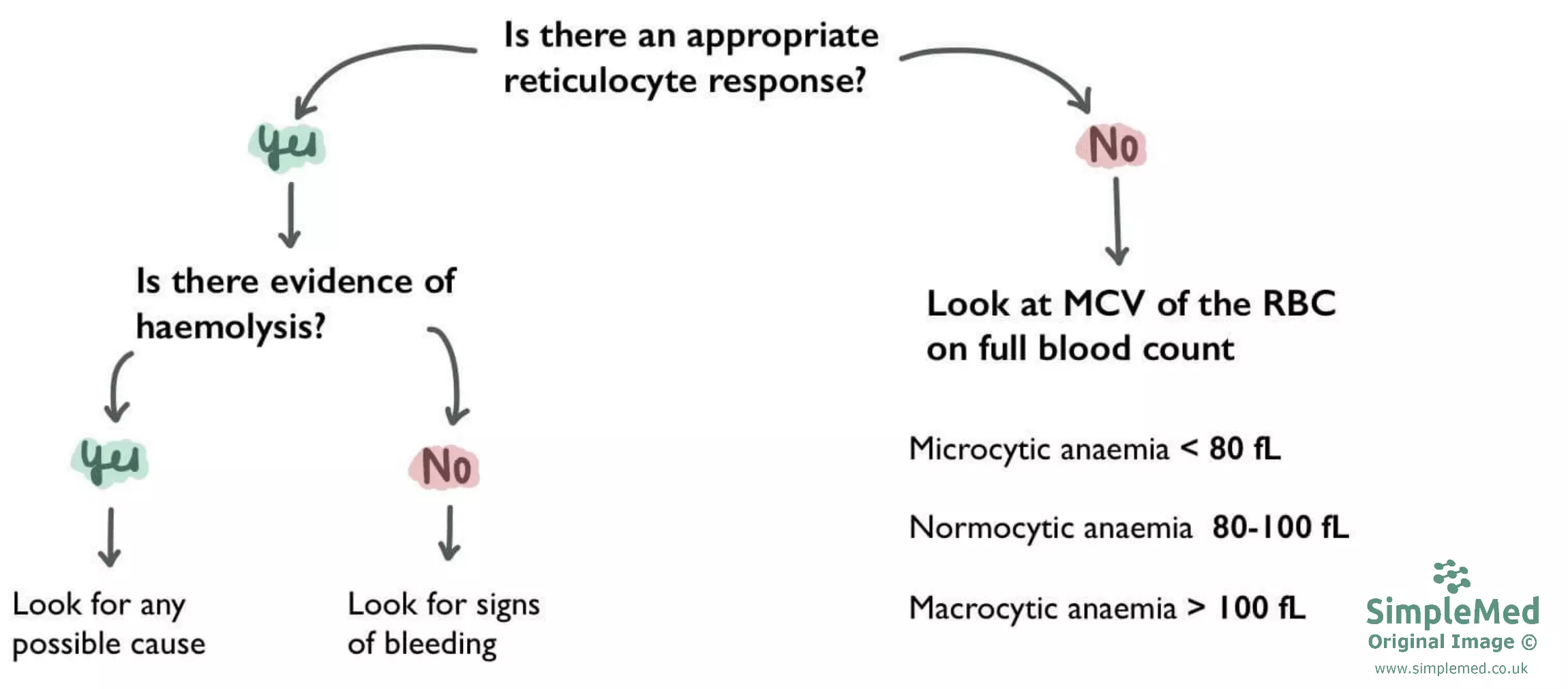
Diagram: A flow diagram showing the classification of anaemia based on reticulocytes and mean corpuscular volume
SimpleMed original by Dr. Keertana Anne
With an appropriate reticulocyte response, reticulocytosis is seen on a blood film (see article on Full Blood Count and Blood Films). This shows an active bone marrow trying to replace lost RBCs rapidly, and is seen in excessive bleeding, splenic sequestration of RBCs and haemolysis.
However, if there is a low reticulocyte count this means the bone marrow is not functioning as normal and will produce abnormal RBCs. You would then look at the mean corpuscular volume (MCV) of cells, which is the average size of RBCs as seen under a blood film.
Microcytic anaemia (Low MCV)
This is characterized by small RBCs. Some causes of this anaemia can be summarized by the mnemonic TAILS:
- Thalassemia
- Anaemia of Chronic Disease (usually seen as normocytic)
- Iron Deficiency Anaemia
- Lead Poisoning
- Sideroblastic Anaemia (a very rare condition in which the body has iron but cannot incorporate it into haemoglobin)
Normocytic anaemia (Normal MCV)
In normocytic anaemia, the size of RBCs is normal, however, the haematocrit and haemoglobin levels are reduced. This can occur due to multiple reasons - the most common being anaemia of chronic disease, associated with chronic infection, inflammatory and malignant disease. This leads to a reduction in serum iron levels, due to a higher amount being taken up by cells. Other causes of normocytic anaemia include, early stage microcytic anaemia (some normal sized cells remain), a combination of microcytic and macrocytic anaemias (red cell distribution width (RDW) will be increased but cell size averages out) renal failure, bone marrow failure and acute blood loss.
Normocytic anaemia is the most common type of anaemia.
Macrocytic anaemia (High MCV)
In macrocytic anaemia, the large size of the RBCs means there is an insufficient number of cells. Causes of this include liver disease, alcohol excess and some types of haemolytic anaemias.
One of the most common types of macrocytic anaemia is megaloblastic macrocytic anaemia. This takes place when the DNA in red blood cells is produced too slowly or not enough. As mentioned above, it is most commonly caused by vitamin B12/folate deficiency.
Anaemia that develops over time may not present with any symptoms as the body can begin to adjust to reduced haemoglobin levels. A rapid decline however can produce more significant symptoms:
- Symptoms - fatigue, pale skin, headache, shortness of breath, palpitations, lack of energy, light-headed/faintness.
- Signs - bounding pulse, postural hypotension, tachycardia.
The way to treat anaemia is by focusing on the underlying cause of it:
- Deficiencies (Vitamin B12/folate/iron) can be treated by increasing levels in the diet or providing the patient with oral supplements. Iron can also be injected if oral absorption is ineffective or slow.
- Find and stop the cause of bleeding - this can be internal bleeding as well as external e.g. in the form of a peptic ulcer.
- If the patient has reduced kidney function, production of the hormone erythropoietin can be stimulated by giving injections (erythropoiesis stimulating agent).
- Blood transfusions can be given in extreme cases.
Edited by: Dr. Ben Appleby
Reviewed by: Dr. Thomas Burnell
- 9338

