Next Lesson - Pelvic Inflammatory Disease
Abstract
- In the UK, the incidence of STIs is increasing leading to increased demand on GUM clinics.
- STIs are passed through contact of mucous membranes, and have a number of risk factors: young adult age, increased number of sexual partners, young age at first intercourse, excessive alcohol or recreational drug use, and lack of access to GUM preventative services.
- Chlamydia infection is caused by Chlamydia trachomatis. Infection can be asymptomatic or present with urethritis and dysuria in men, discharge and dyspareunia in women. If untreated, it can lead to PID or extragenital manifestations such as conjunctivitis and reactive arthritis. It is tested for via swab/urine sample and NAAT, and managed with doxycycline.
- Gonorrhoea is caused by the Neisseria gonorrhoeae bacteria, a Gram negative diplococcus. It commonly can be asymptomatic, but can present with discharge, dysuria or lower abdominal pain in both sexes. If untreated, it can progress to PID. Tested for with swabs/urine samples and NAAT. Treated with IM Ceftriaxone.
- Syphilis is caused by the Treponema pallidum bacteria and has four stages: primary syphilis presents with a chancre (a specific type of ulcer), secondary syphilis with a rash, latent syphilis with no symptoms, and tertiary syphilis with gummata (sores) and neurological symptoms. Treated with penicillin.
- Anogenital warts are caused by HPV strains 6 and 11 (these strains are vaccinated against). The warts can be treated with topical creams or cryotherapy, but HPV infection can persist leading to recurrence of the warts.
- Genital Herpes is caused by Herpes simplex virus (HSV-1 or HSV-2), and presents with painful sores. Acyclovir is the treatment, however, this suppresses symptoms rather than eradicating the virus, and recurrences are common, particularly in the early years after infection.
- Trichomonas vaginalis is a sexually transmitted protozoa which can cause trichomoniasis infection. Usually asymptomatic in men and presenting with a yellow foul smelling discharge that irritates the vulva and vagina in women. It is treated with metronidazole.
- Scabies and pubic lice are parasites that can occur in the genital region.
- Bacterial vaginosis is associated with an imbalance of the normal vaginal flora, often involving overgrowth of Gardnerella vaginalis and other anaerobic bacteria. One of the most common reasons for this is following the disruption of vaginal flora by douching. It presents with offensive ‘fishy smelling’ grey discharge, and is treated by stopping douching and metronidazole.
- Candidiasis or thrush is caused by an overgrowth of the fungus Candida albicans due to immunosuppression, diabetes, COCP or antibiotics. It presents with white, thick discharge and intense itchiness. Management can be difficult due to the nature of the risk factor, anti fungal azoles like fluconazole can help.
- Vaginal discharge is an important symptom of many of these diseases, but it is important to emphasise that some discharge is normal and that it is a change that is valuable in assisting diagnosis.
Core
Infections of the reproductive tract are common in both men and women and have varied causes and aetiologies. Some of these infections can be sexually transmitted.
The sexually transmitted infections HIV and Hepatitis have dedicated own articles in our Infection unit (see HIV and Hepatitis), and so will not be discussed in this article.
Sexually Transmitted Infections (STIs)
In the UK, the incidence of many STIs is increasing (source). This presents a challenge of increased demand on primary care services including GPs and Genitourinary Medicine (GUM) clinics.
STIs are passed on by direct contact of mucosal membranes of an infected person to another person, meaning that STIs can be transmitted by any form of penetrative sex including vaginal, anal or oral sex. As a result sites of infection include the vagina, penis, anus or pharynx.
STIs are most commonly passed on through unprotected sex, which is the performance of sexual acts or sexual intercourse without a barrier method of contraception (e.g. a condom). Condoms are the only form of contraception that both prevents pregnancy and STIs.
Risk Factors:
- Age - STIs are most common in the 15-24 age group.
- Increased Number of Sexual Partners - more chances to come into contact with STIs.
- Lack of Education - individuals who are less well informed may be unaware of the risks of STIs or be unfamiliar with contraception.
- Excessive use of Alcohol or Recreational Drugs - alcohol and recreational drugs are known to impair judgement and lead to more high risk behaviours.
- Lack of Access to Contraception - while condoms are provided free by GUM clinics in the UK, some people are unable to access these.
- Geographic - the clinic might be inaccessible to the individual.
- Stigma - the individual might not want to be seen to attend the clinic due to the stigma sometimes attached to having an STI.
- Education - some people may not know they are provided free.
In the UK, STIs can be managed and treated through a GUM clinic.
With all STIs, the patient should be advised to take part in a thorough screening programme, avoid all sexual contact until the treatment is complete (the duration depends on the infection and regimen), and to take part in contact tracing.
As chlamydia and gonorrhoea are STIs that can be passed very easily between partners who are not using barrier contraception, any patient diagnosed should have their previous partners contacted. In the UK, this is done through an anonymous service provided by GUM clinics in which at-risk parties are contacted via text message and advised to seek screening.
As seen in the table below, asymptomatic infections require a longer period of contact tracing, because with asymptomatic infections, the origin is much harder to establish.
One of the difficulties with contact tracing stems from the fact that not all patients are willing or able to provide the contact information of their sexual partners. Due to confidentiality, patients cannot be forced to give up information they do not have, and patients may not have contact information.
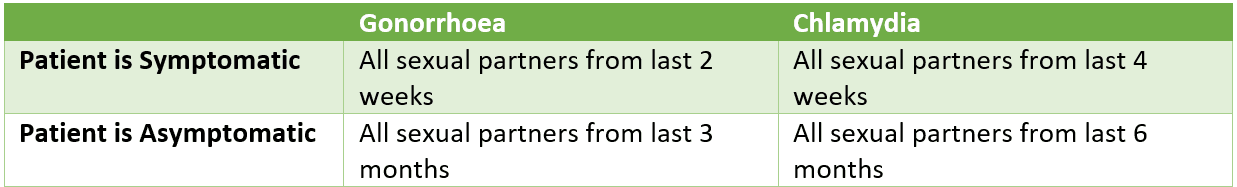
Table - Period of contact tracing
SimpleMed original by Dr. Maddie Swannack
Chlamydia infection is caused by the Chlamydia trachomatis, an obligate intracellular bacteria (meaning it must be inside the cell to replicate). It is classified as a gram negative bacteria although in practice it is difficult to gram stain due to the lack of cell wall. Chlamydia is the commonest STI in the UK (source).
Symptoms
Can be asymptomatic in both sexes, but more likely to be asymptomatic in women.
Men - mild urethritis, dysuria, local inflammation such as epididymitis or prostatitis.
Women - vaginal discharge, dyspareunia (pain on vaginal penetration) or post-coital bleeding.
Complications
If untreated, chlamydia infection can progress to Pelvic Inflammatory Disease (PID) and infertility.
Can also lead to complications outside of the genitals, such as reactive arthritis, urethritis, and uveitis. This can be remembered with the phrase ‘can’t pee, can’t see, can’t climb a tree’ (urethritis, uveitis, reactive arthritis respectively). It is also an important differential diagnosis in a neonate presenting with conjunctivitis, as the bacteria could have been passed on to the child during vaginal birth in an infected mother.
Investigations
As Chlamydia trachomatis cannot be seen on Gram staining, Nucleic Acid Amplification Tests (NAAT) are used to identify it.
The samples are obtained by a vulvovaginal swab in women, and a urine sample in men. Extragenital sites including conjunctiva, pharynx and anus are swabbed if symptomatic or if other non vaginal sex has occurred.
Treatment
The current recommended treatment for chlamydia infection is doxycycline for 7 days, unless contraindicated.
The current recommended treatment pathway can be found here.
Gonorrhoea infection is caused by the bacteria Neisseria gonorrhoeae, a Gram negative, intracellular diplococcus. This means that on Gram staining, it is seen inside the cell as pink circles, arranged in pairs.
Symptoms
Can be asymptomatic in both sexes, but more likely to be asymptomatic in women.
Men - discharge and dysuria.
Women - vaginal discharge and lower abdominal pain.
Due to the similar symptoms to chlamydia differentiation of cause is usually only achieved after NAAT.
Complications
If untreated, gonorrhoea infection has a higher risk of complications than chlamydia. It can lead to PID, and epididymo-orchitis (inflammation of the testes and epididymis).
Investigations
While Neisseria gonorrhoeae does appear on Gram staining, the culturing required takes time. For this reason, NAAT is used, with vulvovaginal or endocervical swabs in women and a urine sample in men.
Treatment
The treatment for gonorrhoea infection is a high dose intramuscular (IM) injection of Ceftriaxone.
The current recommended treatment pathway can be found here.
Syphilis infection is caused by the spirochete (spiral-shaped) Treponema pallidum bacterium. It has a characteristic four stage development if left untreated.
Primary Syphilis
This is the initial stage of a syphilis infection, presenting with a painless ulcer called a chancre at the site of sexual contact. Over the next few weeks, this ulcer will disappear, but during that time the patient is very infectious.
Secondary Syphilis
The secondary stage of a syphilis infection marks the dissemination of the bacteria around the body, and so is characterised by systemic effects: a rash may appear on the body, with a fever, mucosal lesions, weight loss and general malaise.
The patient is still very infectious at this stage, and this may last for up to three months after the initial infection.
Latent Syphilis
Following the secondary stage, the body pushes the disease into latency. At this point, the patient will have no symptoms, and so findings are either incidental, or through the birth of a child with congenital syphilis.
Tertiary Syphilis
This is the most severe stage of syphilis, and it can occur any time from about 1 year after the initial infection and can be as long as 10 years before reactivation of the latent disease. It may never occur if the disease is not reactivated.
The symptoms of this stage of syphilis are severe:
- Gummata - large sores that occur on the skin or on the internal organs.
- Cardiovascular Effects - damage to the heart and blood vessels.
- Neurosyphilis - nervous system damage.
Investigation
Syphilis can be diagnosed either through a blood test or a swab of the primary ulcer if the patient presents at this early stage.
Treatment
The treatment of syphilis is with benzathine benzylpenicillin given in appropriate stage-specific doses.
The current recommended treatment pathway can be found here.
Anogenital warts are a very common viral STI, and are caused by Human papillomavirus (HPV) strains 6 and 11. The current vaccine used for HPV protects against these strains of HPV as well as HPV 16 and 18 which cause cervical cancer.
It typically presents with painless warts on the penis or vulva, but they can appear in the vagina, cervix and perianal skin.
Treatment
There are many treatment options for the appearance of warts.
The first option is to leave them alone: anogenital warts are unsightly and infective, but they can safely be left untreated.
Topical creams are also available to speed up healing, and if needed more intense therapies like cryotherapy (freezing them off) is possible.
However, getting rid of the warts will not get rid of the underlying infection, meaning that the warts can recur many times over a period of up to two years. After this time most people will have cleared the HPV infection, preventing recurrence unless reinfected.
The current recommended treatment pathway can be found here.
Herpes is a viral infection caused by the Herpes Simplex Virus (HSV). There are two divisions of this virus, HSV-1 and HSV-2. Traditionally HSV-1 is associated with oral ulcers and HSV-2 is associated with genital ulcers. However, it has since been shown that both of the virus types can cause both oral and genital ulcers.
Infection with any strain of HSV is especially dangerous in pregnancy, as it can cause neonatal herpes which can be fatal to the newborn child.
Symptoms
Commonly presents with painful ulcers, dysuria or discharge in both men and women. Can be asymptomatic.
It is transmissible in asymptomatic and symptomatic states, but is more infectious with ulceration.
Investigation
Diagnosis is usually clinical, but swabs of ulcers can be taken for viral PCR. Serology has a limited role and is not routinely used for acute diagnosis.
Treatment
Oral acyclovir is the mainstay of treatment for genital herpes. However, it is impossible to cure. This means that while acyclovir can reduce the length of ulceration, there is no way of preventing recurrence. During the first year following symptoms appearing, it is not unusual to have 5 recurrences within the year, and this may continue lifelong.
Lifestyle modifications might also aid in relieving the symptoms associated with the ulceration, such as using an emollient such as Vaseline, and avoiding sharing towels with other family members.
The current recommended treatment pathway can be found here.
A sexually transmitted protozoal infection caused by Trichomonas vaginalis.
Symptoms
Men - often asymptomatic but can cause dysuria or discharge.
Women - typically yellow vaginal discharge that irritates the vulva and vagina, has a foul smell and may be frothy in appearance.
Investigation
High vaginal swabs in women and urine samples in men are tested using nucleic acid amplification tests for diagnosis.
Treatment
Oral metronidazole is the treatment of choice for Trichomonas vaginalis.
The current recommended treatment pathway can be found here.
Other Infections of the Genitourinary Tract (Non-Sexually Transmitted Infections)
This section of the article is dedicated to infections of the reproductive tract that are not necessarily always transmitted sexually.
Scabies and pubic lice are small parasites that cause irritation of the skin. They can occur around the genital region or in any other region of skin and are passed through contact with infected skin, shared towels or bedsheets.
This vaginal infection is commonly caused by Gardnerella vaginalis but can be caused by many other anaerobic bacteria. It is caused by an imbalance in the normal flora of the vagina. Any practice that disrupts the vaginal flora and the normal pH of the vagina, including douching and washing inside the vagina, can cause the condition although the specific pathophysiology is unclear. Although not an STI itself it can increase the risk of contracting an STI.
Symptoms
Offensive smelling discharge that is often greyish in colour, but not associated with pruritus or pain.
Investigation
Diagnosis is usually clinical, supported by vaginal pH testing and/or microscopy. Routine culture is not recommended.
Treatment
Oral metronidazole is the treatment of choice, as well as curtailing any risky practices such as douching.
The current recommended treatment pathway can be found here.
Vulvovaginal Candidiasis (Thrush)
This fungal infection of the vagina is commonly caused by Candida albicans and has multiple risk factors including immunosuppression (e.g. HIV infection, pregnancy), diabetes (sugar in the urine encourages fungal growth), recent antibiotics (kill the local flora) and possibly the combined oral contraceptive pill (COCP), although evidence for this association is limited. Thrush can also present orally and is a common finding in elderly patients.
Symptoms
White, thick, non-offensive discharge associated with severe pruritus, pain and often dyspareunia.
Investigation
Investigation is not usually required in uncomplicated cases. High vaginal swabs may be considered if symptoms are recurrent, severe, or do not respond to treatment.
Treatment
Management of thrush can be tricky, especially if the precipitating risk factors cannot be treated. Thrush can often present as a recurring problem.
Treatment can be through creams, pessaries or oral antifungals of the -azole class like the oral treatment fluconazole.
The current recommended treatment pathway can be found here.
Vaginal discharge is a common initial presentation of many of these diseases. It is therefore important to understand the different types of vaginal discharge as this will assist in achieving a diagnosis.
Vaginal discharge is normal, and it is normal for it to vary slightly in texture or amount throughout the menstrual cycle. It is important to emphasise that it is the change from normal for that patient that is a cause for concern.
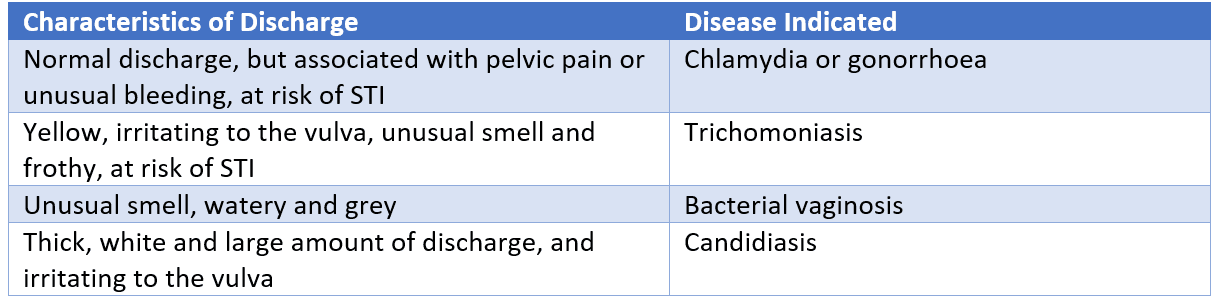
Table - The characteristics of vaginal discharge and the possible conditions associated with that presentation
SimpleMed original by Dr. Maddie Swannack
While the above table can be helpful in practice, it is also important to include the rest of the clinical picture when making a diagnosis.
All recommended up-to-date treatment pathways can be found on the website https://cks.nice.org.uk/ and were as listed on 01/07/2020.
Edited by: Dr. Ben Appleby
Reviewed by: Dr. Thomas Burnell
- 4726

