Next Lesson - Pneumonia and Other Lower Respiratory Tract Infections
Abstract
- Chronic Obstructive Pulmonary Disease (COPD) is characterised by airflow limitation that is not fully reversible, and is an umbrella term that encompasses both emphysema and chronic bronchitis.
- Emphysema is a condition in which there is destruction of the terminal bronchioles and distal air spaces, through the breakdown of elastin, leaving lungs with very little surface area.
- Chronic bronchitis is a condition that occurs frequently in smokers, in which there is hypersecretion of mucus, leaving narrowed bronchi.
- COPD has a gradual onset and usually presents in older people with a long history of smoking, but can also present in non-smokers. Symptoms include a morning cough that is usually productive and shortness of breath.
- COPD is investigated via spirometry, which demonstrates persistent airflow obstruction, and a chest x-ray to help exclude alternative diagnoses.
- Management focuses on symptom control and is achieved through medication and managing lifestyle factors. COPD cannot be cured.
- An acute exacerbation of COPD is an event characterised by a sustained increase in the patient’s day-to-day symptoms, that is beyond normal variants and acute in onset. Exacerbations can be infective or non-infective.
Core
Chronic Obstructive Pulmonary Disease (COPD) is characterised by airflow obstruction that is not fully reversible, and is an umbrella term that encompasses both emphysema and chronic bronchitis. The airflow limitation is usually progressive (meaning that it cannot be cured or reversed). It is estimated that 1.2 million people in the UK live with COPD (source).
The primary cause of COPD is smoking, meaning that most patients diagnosed with COPD will have a significant smoking history.
However, it is important to remember that other causes of COPD do exist, including air pollution, occupational exposure to certain chemicals, and inherited conditions such as alpha-1 antitrypsin deficiency.
Emphysema is a condition in which destruction of the terminal bronchioles and distal air spaces occurs, through the breakdown of elastin, a key component in alveolar walls. This breakdown leads to loss of integrity of the alveolar walls, and destruction of the surrounding small airways, meaning that all air spaces distal to the terminal bronchioles are permanently enlarged into useless spaces called bullae.
During expiration, when the pressure outside the airway rises, the smaller airways collapse due to the lack of surrounding elastic tissue keeping them patent, causing airway obstruction. The loss of elastic tissue in the lungs also causes them to hyperinflate, as the elastic recoil of the lungs has been destroyed.

Image - Lung taken from a cadaver where the patient had emphysema, showing an example of the bullae
Creative commons source by Yale Rosen [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Chronic bronchitis is a condition that occurs frequently in smokers, in which there is hypersecretion of mucus caused by inflammation of the large airways. There is also ciliary dysfunction, meaning that the normal clearance mechanisms for mucus are not effective. This means that patients with chronic bronchitis have a chronic productive cough, and are more prone to have frequent respiratory tract infections. The remodelling and narrowing of the airways caused by the inflammation causes irreversible airflow obstruction.
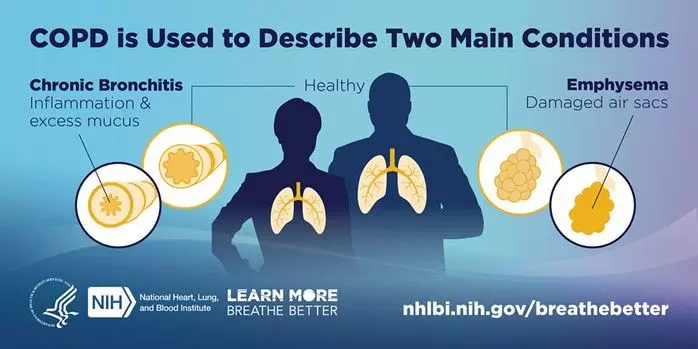
Diagram - Components of COPD, with chronic bronchitis on the left and emphysema on the right. It shows the differences between healthy bronchi and air sacs, and those seen in COPD
Public Domain Source by National Heart, Lung, and Blood Institute, NIH [Public domain]
The airway narrowing and destruction of lung tissue predisposes patients with COPD to hypoxia, particularly during physical activity. This progressive hypoxia causes pulmonary vasoconstriction (to maintain the ventilation/perfusion ratio) and over time, leads to vascular smooth muscle thickening, with subsequent pulmonary hypertension.
A patient with COPD usually has features of both emphysema and chronic bronchitis, and both conditions are progressive and not reversible. To summarise, the changes that occur as a result of COPD to the airways include:
- Enlargement of the mucus-secreting glands of the central airways leading to increased mucus production and a predisposition to infection in the mucus.
- Replacement of ciliated cells with goblet cells, and dysfunction of the ciliary cells that remain leading to stasis of the already increased amount of mucus.
- Breakdown of elastin, causing destruction of alveolar walls and their structure leading to the formation of large air spaces, reducing the total surface area available for gas exchange.
- Vascular bed changes leading to pulmonary hypertension.
- Loss of elastic recoil.
COPD has a gradual onset and usually presents in older people with a long history of smoking. That being said, it can have other causes, and so a presentation typical of COPD without a smoking history should be investigated for other causes, such as alpha-1 antitrypsin deficiency. A cough is usually the first symptom of COPD, which begins as a morning cough but becomes constant as the disease progresses. It is usually productive, and the sputum quality and quantity may change with exacerbations and superimposed infections.
Shortness of breath usually occurs on exertion at the start of the disease process but may progress to occurring at rest.
The MRC dyspnoea score is used to grade how severe a patient is experiencing breathlessness, ranging from 1 (not troubled by breathlessness unless exercising strenuously) to 5 (too breathless to leave the house, or gets breathless when dressing or undressing).
The physical signs of COPD include:
- Tachypnoea, as the patient tries to compensate for the hypoxia
- Visible use of accessory muscles (e.g. sternocleidomastoid or trapezius) as the patient experiences difficulty moving air in and out of the lungs
- Barrel chest, an increased diameter of the chest due to hyperinflation and incomplete expiration
- Hyper-resonance on percussion of the chest due to hyperinflation
- Decreased breath sounds and reduced air entry
- Pursed-lip breathing
- Potential wheeze
Signs of late COPD include:
- Flapping tremor of the hands, caused by hypercapnia
- Central cyanosis, due to hypoxia
- Signs of right-sided heart failure, such as distended neck veins and ankle oedema, secondary to pulmonary hypertension
When investigating COPD, spirometry is used. It will show an obstructive pattern, where the forced expiratory volume in one second (FEV1) compared to the forced vital capacity (FVC), the FEV1/FVC ratio, is less than 70%, due to the reduced FEV1. This is the same pattern as seen in patients with asthma, however, in patients with COPD the airflow obstruction is not fully reversible following treatment with bronchodilators. A vitalograph (or flow volume loop) will show the typical obstructive pattern of scalloping.
How well a patient performs on spirometry can be used to grade their severity of airway obstruction:
- Mild airflow obstruction = FEV1 80% or more of predicted.
- Moderate airflow obstruction = FEV1 50-79% of predicted.
- Severe airflow obstruction = FEV1 30-49% of predicted.
- Very severe airflow obstruction = FEV1 less than 30% of predicted.
The predicted value for spirometry is based on a patient’s gender, age and height.
The most useful piece of imaging to diagnose someone with COPD is a chest x-ray. The chest radiograph will show signs of hyperinflation, such as a flattened diaphragm and an increased antero-posterior diameter of the chest, which is present if an increased number of ribs can be seen within the lung fields on a standard chest radiograph, reflecting lung hyperinflation.
A chest x-ray may also be signs of complications, such as the presence of infiltrates consistent with pneumonia or a pneumothorax. A chest x-ray is also useful for excluding other diagnoses in patients with a chronic cough, such as lung cancer.
A high-resolution CT scan is useful for providing an accurate assessment of the alveolar destruction caused in emphysema, which may be useful if there is uncertainty surrounding the diagnosis, or if surgical intervention is required, but is not routinely used in diagnosing COPD.

Image - Chest x-ray of a patient with COPD, showing signs like a flattened diaphragm, 8 ribs visible within the lung fields, and the typical ‘barrel chest’ appearance
Creative commons source by Mikael Häggström, M.D [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Pulse oximetry and/or arterial blood gas analysis can be carried out in acutely unwell patients to assess for hypoxia, respiratory failure and hypercapnia.
Alpha-1 antitrypsin level may be checked if there is high suspicion of deficiency, such as a positive family history and atypical COPD history, such as a young, non-smoker presenting with COPD symptoms.
The treatment for COPD is mainly focused on managing symptoms, and is achieved through a mixture of making lifestyle changes and medication. These are the mainstay of treatments, because the disease process of COPD involves destruction of alveolar walls, and scarring of the airways, neither of which can be reversed.
Stopping smoking is the main lifestyle change a patient can make to reduce their symptoms. This is because smoking can irritate the already-inflamed lining of the lungs, and can further contribute to ciliary dysfunction, which increases the risk of exacerbations of COPD.
They can also attend pulmonary rehabilitation, a supervised exercise programme which aims to increase the patient’s exercise tolerance, educate them on the disease and give them nutritional advice. This helps to improve symptoms, exercise capacity and quality of life, so patients can live with fewer symptoms for longer.
Stable COPD therapy includes a range of medication, such as bronchodilators, anticholinergics, inhaled steroids and antimuscarinics. These medications aim to reduce the day-to-day symptoms that a patient experiences.
Patients with COPD should also be given annual flu vaccines and appropriate pneumococcal vaccination in line with current UK guidance, to help prevent further infections. Patients with frequent exacerbations despite optimal inhaled therapy may be considered for prophylactic antibiotics under specialist supervision, to help reduce recurrent infective exacerbations.
Long term oxygen therapy at home for at least 16 hours a day has been shown to improve survival by reducing hypoxia, but this is a very intense undertaking for the patient, and for the patient to be safe to have oxygen tanks in their home they must meet certain criteria.
The last step in treatment for COPD is surgical intervention, with procedures such as removal of bullae, lung volume reduction and lung transplants. They are used to improve lung dynamics, exercise adherence, and quality of life. However, these surgeries are not often performed, as patients are often not well enough with other co-morbidities to undergo surgery.
An acute exacerbation of COPD is an event characterised by a sustained increase in the patient’s day-to-day symptoms, that is beyond normal variants and acute in onset. These can be infectious or non-infectious, and typically present with acute worsening of shortness of breath, cough and sputum production, with fever sometimes present in infective cases.
Management of acute COPD exacerbation includes:
- Monitoring for hypoxia and hypercapnia using pulse oximetry and arterial blood gas analysis.
- Appropriate antibiotics when there is evidence of bacterial infection, particularly to cover Haemophilus influenzae and Streptococcus pneumoniae.
- Nebulised bronchodilators.
- Oral steroids - a short course of high dose oral prednisolone.
- Controlled oxygen therapy with close monitoring, aiming for target oxygen saturations in line with COPD guidance, while keeping under review for CO2 retention.
- Possible escalation to non-invasive ventilation (e.g. BI-PAP) for worsening type 2 respiratory failure.
- Intensive treatment unit (ITU) referral for invasive ventilation may be considered if repeated ABG shows no signs of improvement with inpatient management.
COPD is a condition that is not reversible, and the progressive damage to the lungs predisposes the patients to a number of conditions:
- Recurrent infection, possibly progressing to pneumonia
- Pneumothorax
- Respiratory failure
- Right sided heart failure
Edited by: Dr. Maddie Swannack
Reviewed by: Dr. Thomas Burnell
- 6538

