Next Lesson - Upper Gastrointestinal Tract Pathology
Abstract
- The hindgut is defined as the section of the gut from two-thirds of the way along the transverse colon to the anal canal.
- The hindgut's arterial blood supply is by the inferior mesenteric artery, its venous drainage by the inferior mesenteric vein, and it is innervated by sympathetic lumbar splanchnic nerves and parasympathetic pelvic splanchnic nerves (S2-S4).
Core
The hindgut gives rise to the distal 1/3 of the transverse colon, the descending colon and the sigmoid colon, and these are sections of the large intestine that lie in the left half of the abdominal cavity.
The transverse colon is an intraperitoneal structure and has its own mesentery, the transverse mesocolon.
The descending colon is a retroperitoneal structure, but it lies anterior to the left kidney. Its arterial supply is from the left colic artery which branches off the inferior mesenteric artery (IMA) and its venous drainage is into the left colic vein then into the inferior mesenteric vein (IMV). Lymphatic drainage is into the inferior mesenteric lymph nodes.
The sigmoid colon has its own mesentery (the sigmoid mesocolon) and is an ‘S’ shaped section of the large intestine proximal to the rectum. Its arterial supply is from the sigmoid arteries which branch off the IMA and its venous drainage is into the sigmoid veins then into the IMV. Lymphatic drainage is into the inferior mesenteric lymph nodes.
The colon is much wider and shorter than the small intestine, and it has crypts not villi. The external longitudinal muscle of the colon is incomplete - it is made up of teniae coli (bands of muscle) which cause the formation of haustra (sacculations) when they contract. These can be differentiated from the plicae circularis of the small intestine because the plicae circularis traverse the whole diameter of the lumen, and the haustra do not.
The main functions of the colon are final water and electrolyte absorption (facilitated by eNaC channels which move sodium from the lumen into the enterocytes), and formation and temporary storage of faeces prior to defaecation.
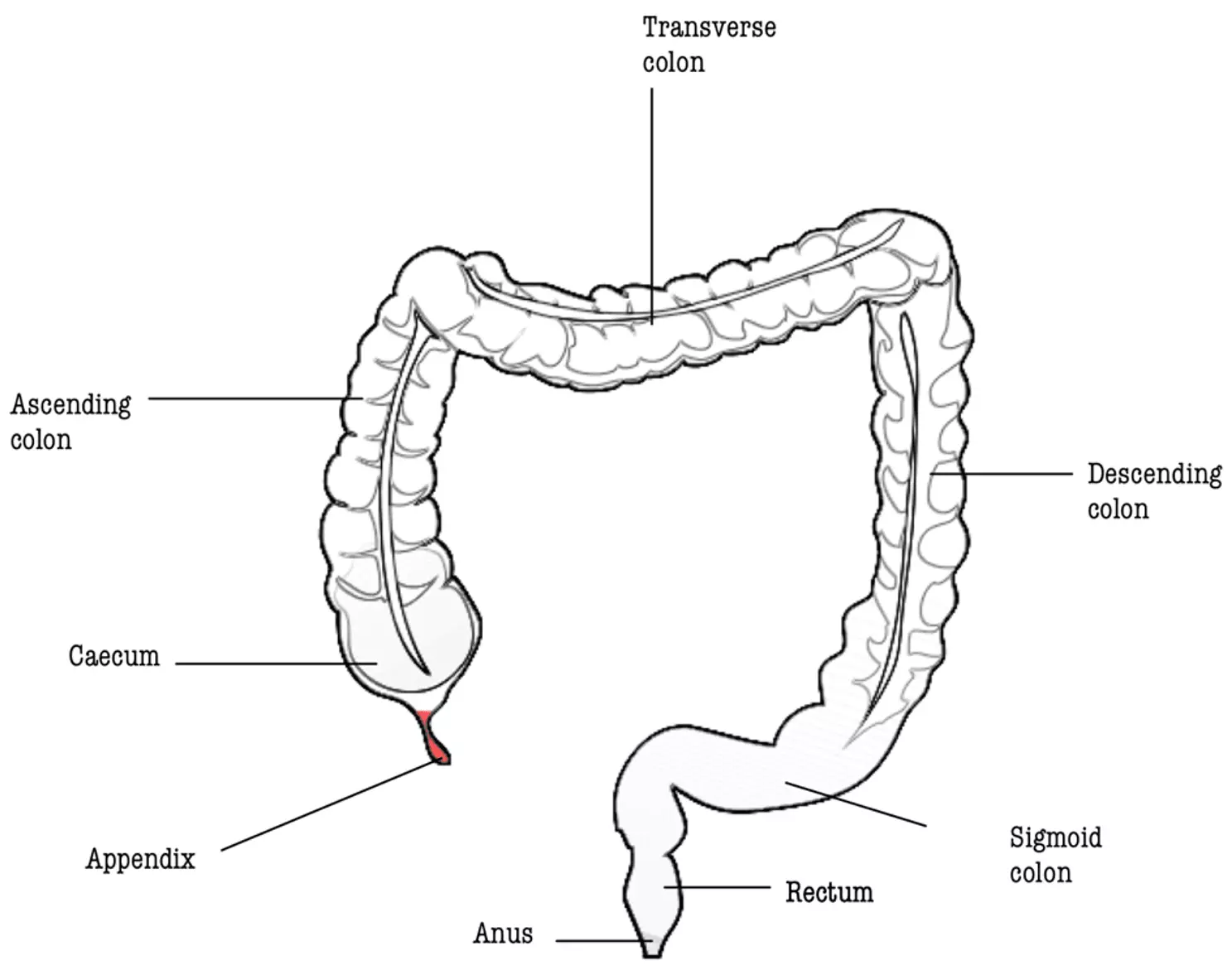
Diagram - The anatomy of the large intestine
Public Domain Source by Mikael Häggström and B jonas, edited by Dr. Laura Hansell [Public domain]
The rectum has a curved shape and sits anteriorly to the sacrum in the pelvis. It is distinguishable from the sigmoid colon because it has a continuous band of longitudinal muscle instead of the intermittent teniae coli like the colon.
It is split into thirds. The upper third is intra-peritoneal, the middle third retroperitoneal, and the lower third has no peritoneum as it sits below the peritoneal cavity.
The upper third of the rectum’s arterial supply is the superior rectal artery which branches off the IMA and its venous drainage is into the superior rectal vein then into the IMV. Lymphatic drainage is into the pararectal lymph nodes then into the inferior mesenteric nodes.
The middle third of the rectum’s arterial supply is the middle rectal artery which branches off the internal iliac artery and its venous drainage is into the middle rectal vein then into the internal iliac vein. Lymphatic drainage is a combination of the upper and lower third’s drainage.
The lower third of the rectum’s arterial supply is the inferior rectal artery which branches off the internal pudendal artery and its venous drainage is into the inferior rectal vein then into the internal iliac vein. Lymphatic drainage is into the internal iliac lymph nodes.
The combination of the portal (upper third drains into IMV and so enters the portal system) and systemic (lower two-thirds drain into the internal iliac vein and so enters the systemic system) venous drainage of the rectum results in a portosystemic anastomosis. This anastomosis is important because it means that if the portal system becomes damaged in the future (for example due to liver cirrhosis), the blood can join the systemic circulation at this point.
The function of the rectum is the temporary storage of faeces prior to defaecation. Stretching of the rectum is what stimulates the urge to open the bowels.
The anal canal is the distal end of the gastrointestinal tract - it begins at the terminal rectum and ends with the anus.
The canal is divided into two sections by a line known as the pectinate line or the dentate line. Above this line, the anal canal is developed from the hindgut, and below this line the anal canal is developed from the proctodeum, an embryological structure formed by the folding of the embryo. For more information, please see our article Development of the Gastrointestinal Tract (here).
Above the pectinate line, the anal canal’s arterial supply is the superior rectal artery which branches off the IMA and its venous drainage is into the superior rectal vein then into the IMV. This means that the superior portion of the anal canal drains into the portal system. Lymphatic drainage is into the internal iliac lymph nodes. The epithelium of the anal canal above the pectinate line is columnar (glandular) epithelium and it has a visceral nerve supply (S2,3 and 4) that allows for a sense of stretch.
Below the pectinate line, the anal canal’s arterial supply is the inferior rectal artery which branches off the internal pudendal artery and its venous drainage is into the inferior rectal vein then into the internal pudendal vein. This means that the inferior portion of the anal canal drains into the systemic circulation. Lymphatic drainage is into the superficial inguinal lymph nodes. The epithelium of the anal canal below the pectinate line is stratified squamous epithelium and it has a somatic nerve supply (S2,3 and 4) that allows for a sense of pressure, pain, and temperature.
The functions of the anal canal are faecal continence and defaecation, which are controlled by sphincters.
Diagram - The anatomy of the anal canal
Public Domain Source by U.S. Government National Institutes of Health [Public domain]
Edited by: Dr. Maddie Swannack
Reviewed by: Dr. Thomas Burnell
- 1407

