Next Lesson - Puberty
Abstract
- The gonads begin development as an indifferent part of the urogenital ridge and a collection of germ cells. The SRY gene unique to the Y chromosome is key in determining sex. The presence of the SRY gene results in the formation of the seminiferous tubule including Sertoli cells (produce anti-Mullerian hormone) and Leydig cells (which produce testosterone). Without the SRY gene, ovaries form.
- The Mesonephric (Wolffian) and the Paramesonephric (Mullerian) ducts form the common basis of the internal genitalia. With the release of testosterone and anti-Mullerian hormones in the male, the mesonephric ducts persist and the paramesonephric ducts degenerate. Without these hormones in the female, the paramesonephric ducts persist, and the mesonephric ducts degenerate.
- The external genitalia of embryos up to 9 weeks old are undifferentiated. Under the influence of testosterone, the genital tubercle grows into the glans penis, pulling the urethral folds to form the shaft. The genital swellings fuse and become the scrotum. Without testosterone, the genital tubercle grows only slightly into the clitoris, and the urethral folds and the genital swellings form the labia minora and majora respectively.
- The gubernaculum is a fibrous structure that guides the gonads into their proper position. In males, it pulls the testicles from the abdomen into the scrotum and is then known as the scrotal ligament. In females, it attempts to pull the ovaries down similarly to the testicles, but is blocked by the forming uterus. It then degenerates to form the ovarian ligament and the round ligament.
- Increased levels of testosterone in females or insensitivity to testosterone in males can lead to abnormalities forming the internal and external genitalia.
Core
The development of the reproductive and urinary systems overlap greatly due to their close proximity and common features. They both develop from the urogenital ridge, a structure made of mesoderm that develops from intermediate mesoderm along the posterior abdominal wall, adjacent to the developing dorsal body wall, as the trilaminar disk undergoes folding around week 4 of development.
The important thing to remember when considering the formation of the internal and external genitalia is that developmentally, both sexes start the same, and which structures persist is determined by hormones.
The development of the gonads is the first key step in the development of the reproductive system and dictates the development of the rest of the internal and external genitalia of the embryo. The gonads begin as an indifferent stage meaning that at first, they are the same in male and female embryos. The gonads develop from the urogenital ridge, a pair of longitudinal ridges derived from mesoderm and germ cells, which have migrated from the yolk sac to the urogenital ridges. At the same time, the epithelium of the urogenital ridge penetrates the mesoderm layer to form primitive sex cords. These primitive sex cords and the germ cells together form the indifferent gonad.
Whether the indifferent gonads develop into testes or ovaries depends on the presence of the SRY gene. This gene is found only on the Y chromosome, meaning that only males with the sex chromosomes XY will express the SRY gene, and that females with the sex chromosomes XX will not.
The SRY gene prompts the primitive sex cords to develop the structure of a testicle, forming the medullary cords of the testicle, which will develop into the sperm-producing seminiferous tubules after puberty. The seminiferous tubules are lined with Sertoli cells, which produce a hormone called Anti-Mullerian Hormone (this influences internal genitalia development as described below). In between these tubules are Leydig cells, which start to produce testosterone at around 8 weeks of gestation. It is this testosterone production that determines the formation of both internal and external features of the genitals.
If no SRY gene is present, the primitive sex cords degenerate, allowing the epithelium of the indifferent gonad to develop into a structure called cortical cords. These break up around three months into the pregnancy, surrounding each of the germ cells with an epithelial layer, forming them into primordial follicles (a precursor to oocytes or egg cells).
In summary: with the SRY gene found on the Y chromosome, the primitive sex cords and germ cells form a testis, which will begin to produce testosterone. Without the SRY gene, the primitive sex cords and germ cells form an ovary.
In the first few weeks of development, the cloaca is an outpouching of the hindgut. It is the site at which the bladder, rectum, and a series of ducts will open onto as development continues. At this early point it is covered by a membrane, and so is not open.
The two ducts that sit in the cloaca are:
- The Mesonephric (Wolffian) Duct - this connects the embryonic kidney (mesonephros) with the cloaca.
- The Paramesonephric (Mullerian) duct - a duct which runs alongside the mesonephric duct which is open at the top.
These ducts have specific roles within the development of the male and female reproductive tracts.
Testosterone, which has been produced by the Leydig cells of the testes, acts on the mesonephric ducts to form the vas deferens and the epididymis.
Anti-Mullerian hormone, produced by the Sertoli cells of the testes, acts on the paramesonephric ducts and causes them to degenerate.
In a nutshell - The mesonephric duct forms the internal male genitalia.
In the female, there are no Leydig cells to produce testosterone. Without the influence of testosterone, the mesonephric ducts degenerate.
Furthermore, as there are no Sertoli cells to produce anti-Mullerian hormone the paramesonephric ducts do not degenerate. As a result, they continue to develop, forming the uterus, fallopian tubes, and upper part of the vagina.
The lower part of the vagina is formed by a part of the urogenital sinus, which fuses with the paramesonephric ducts to complete the vagina.
In a nutshell - the paramesonephric duct forms the internal female genitalia.
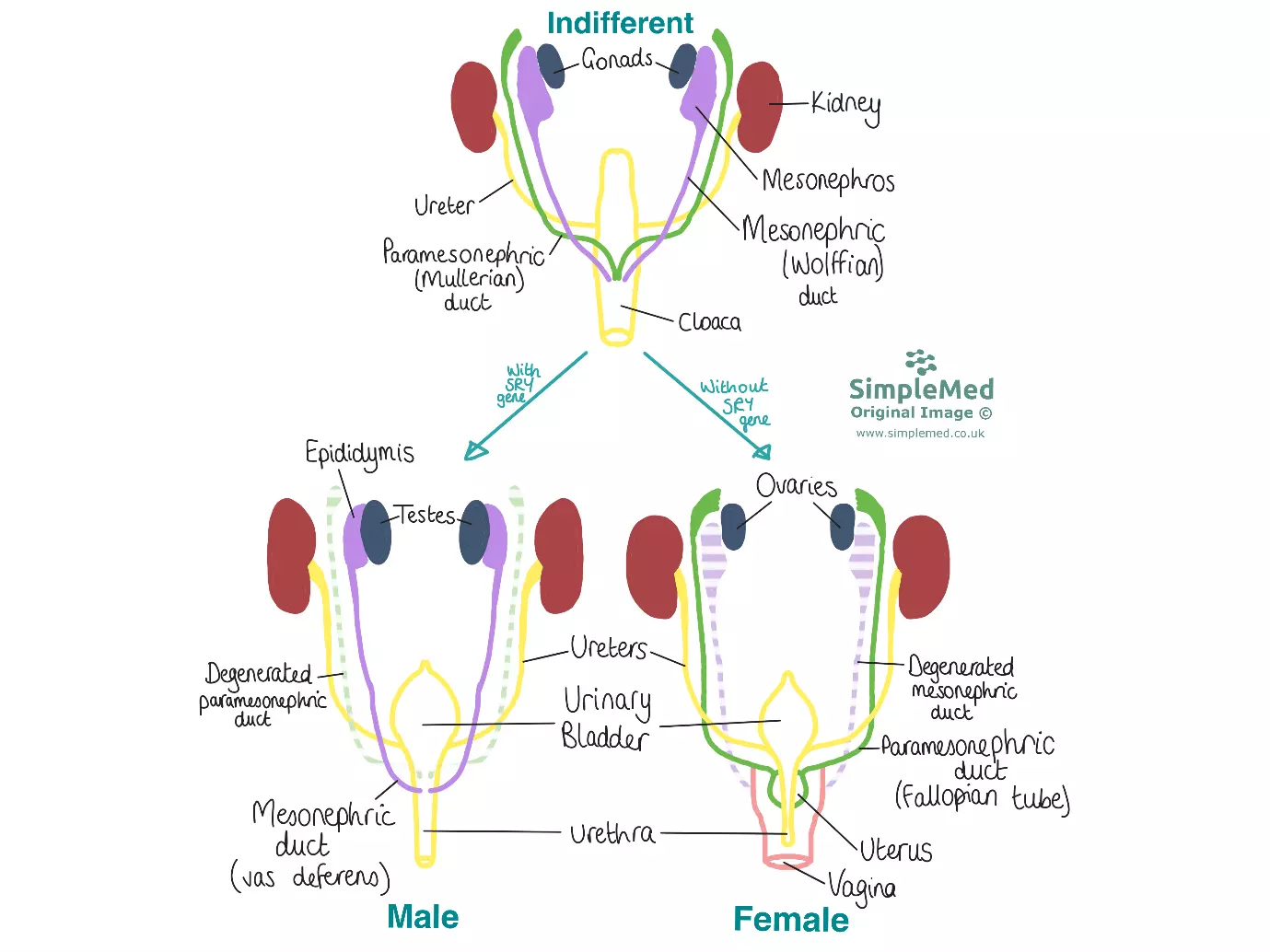
Diagram - The differences between the development of the internal genitalia of the male and the female as viewed in the coronal plane
SimpleMed original by Dr. Maddie Swannack
Until around 9 weeks of gestation, the external genitalia of male and female embryos are identical. Up until this point, the genitalia have been developing as part of the cloacal membrane.
Earlier in development, mesenchymal stem cells migrated from the primitive streak to the cloacal membrane, to form two cloacal folds. These folds fuse to form the genital tubercle and the urethral folds. Genital swellings develop either side of the urethral folds.
Testosterone is produced by the Leydig cells of the testis and is converted to dihydrotestosterone (DHT), which drives the development of the external genitalia of the male.
The genital tubercle grows rapidly, elongating to form the glans penis. The urethral folds are pulled with it, forming the shaft of the penis, and the two folds fuse at around 4 months of gestation to form the urethra.
This step of development is clinically relevant, because failure of this fusion can lead to hypospadias. Hypospadias is a condition in which the opening of the urethra is not at the end of the penis, but somewhere along the caudal aspect.
The genital swellings move caudally and fuse, becoming the scrotum.
In the female, there are no Leydig cells to produce testosterone. This means that the genital tubercle does not undergo rapid elongation to become the penis, but instead grows slightly to become the clitoris.
Without the elongation of the genital tubercle, the urethral folds do not stretch and fuse, and go on to form the labia minora.
Without the development of the penis, the genital swellings do not need to move caudally, so remain where they are and develop into the labia majora.
The gubernaculum is the fibrous structure that pulls the gonads from the lumbar region where they form into their correct position. It does this by having one end attached to the gonad, and the other to the genital swellings (precursors to the scrotum or the labia majora). The ‘correct’ position varies between male and female, with the testicles ending up in the scrotum, and the ovaries ending up in the pelvis.
As the embryo grows, the gubernaculum stays the same length and as a result provides traction on the testes. It guides the testes through the inguinal canal and into the scrotum.
As the testes descend, they retain their original blood and lymphatic drainage, which is also extended during their descent. As a result, the testes have a curious vascular and lymphatic supply. The testicular arteries insert into the abdominal aorta and as a result, have a rather long course through the pelvis. Likewise, the lymphatic drainage of the testes is curious, as they drain into the para-aortic lymph nodes.
The gubernaculum remains postnatally as the scrotal ligament.
The ovaries have a very similar path to the testes, and again retain their blood and lymphatic supply from their original position.
However, the ovaries are stopped in their descent by the developing uterus, which prevents the gubernaculum from pulling the ovaries into the inguinal canal.
Instead, the gubernaculum fuses with the uterus and degenerates, forming two ligaments. The ovarian ligament, which attaches the ovary to the uterus, and the round ligament connects the uterus to the labia majora.
Issues with the Development of Genitalia
As with the development of any organ system, the complexity of the process leaves plenty of chance for error. In the genitalia, these errors often occur due to improper hormone levels.
Increased Testosterone in the Female Embryo
If there is a high level of testosterone in an XX fetus, for example due to excess androgen exposure during development, both ducts will be retained.
Because this embryo is XX, it has no Y chromosome and therefore no testicles to produce anti-Mullerian hormone, meaning the paramesonephric ducts will remain and develop as normal.
However, with the increased testosterone, the mesonephric ducts, in full or in part, will be maintained and develop.
This means that this embryo will develop with both ducts still present, which can lead to problems with the function of the uterus, as there will be remnants of the mesonephric duct still present.
Androgen Insensitivity Syndrome
Androgen insensitivity syndrome is a condition that affects fetuses with the XY genotype. These fetuses have a Y chromosome that carries the SRY gene, so testes will develop normally and release the normal amount of testosterone (an androgen). However, the receptors for testosterone are not functioning properly, meaning the embryo is not ‘sensitive’ to the testosterone. This means that the mesonephric ducts do not develop where they should, because the faulty receptor does not respond to the testosterone in effect developing as if no testosterone has been released i.e. along the lines of female development.
However, because the testes are functioning normally, they produce anti-Mullerian hormone, meaning the paramesonephric ducts degenerate as would be normal in a male.
This results in an embryo that has the XY genotype and no uterus due to the degeneration of the paramesonephric ducts, but due to the lack of response to testosterone, will have the external genitalia of a female. As a result children with this condition are often assigned a female gender at birth due to their phenotype.
Edited by: Dr. Ben Appleby
Reviewed by: Dr. Thomas Burnell
- 7082

