By Dr. Thomas Burnell and Dr. Bethany Turner
Next lesson - Control of Cardiac Output
Abstract
- There are two types of blood flow within a blood vessel: laminar and turbulent.
- From feeling a pulse, you can determine its rhythm, rate and character. Abnormal pulses include bounding, thready, regularly irregular, irregularly irregular, bradycardic and tachycardic. These can indicate pathology.
- The mean arterial pressure can be calculated by MABP = 1/3 systolic P + 2/3 diastolic P or MABP = diastolic + 1/3 pulse pressure.
- A raised JVP indicates a raised venous pressure which can be a sign of pathology in certain conditions.
Core
Blood flow within a vessel can be described in two ways, either laminar or turbulent:
- Laminar flow is where all the blood is flowing in one direction within a blood vessel. The blood flowing in the centre of the blood vessel is flowing faster than the blood closer to the edge (a parabolic profile). This can be thought of as circular layers of blood in a vessel following at different speeds.
- Turbulent flow is where the blood is flowing in different directions and it’s all a bit chaotic. This occurs when:
- Blood passes an obstruction, e.g. stenosis.
- Blood passes over rough surface, e.g. atherosclerosis.
- Resistance to blood flow is increased, e.g. hypertension.
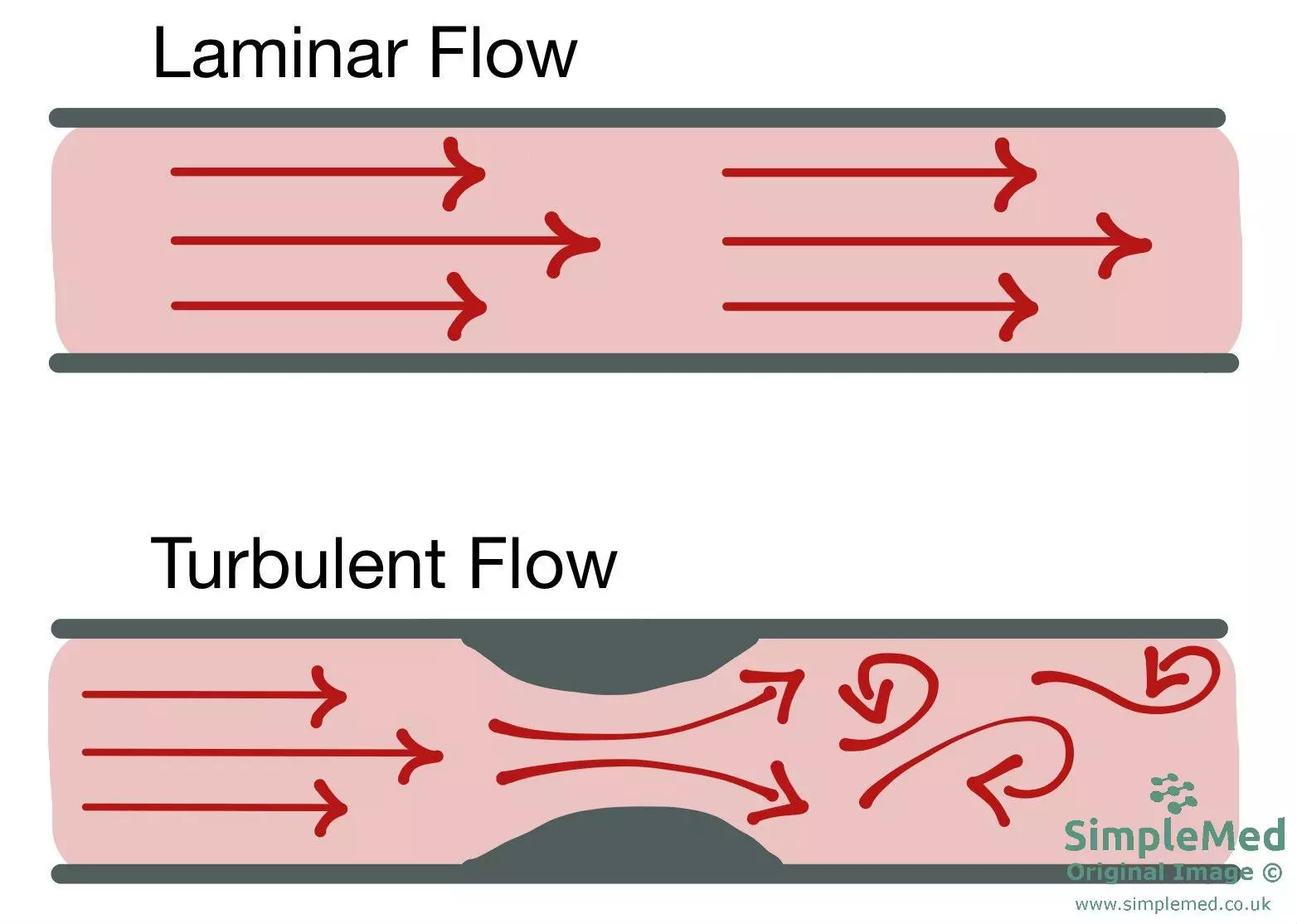
Diagram - Diagrammatic depiction of both laminar and turbulent blood flow - the arrows represent separate blood flow streams. In the second diagram, after the obstruction the flow becomes turbulent
SimpleMed original by Dr. Thomas Burnell and Dr. Bethany Turner
When feeling a pulse, we feel the pressure wave being transmitted before the blood arrives.
Type of pulse rhythm:
- Regular - lub dub lub dub...
- Regularly irregular - the beat is abnormal but the pattern is repeated at set intervals. E.g. 2nd degree heart block.
- Irregularly irregular - the beat is abnormal and does not follow a pattern. E.g. ventricular/atrial ectopics and atrial fibrillation.
Type of pulse rate:
- Bradycardia - where the heart rate is less than 60 beats per minute.
- Tachycardia - where the heart rate is more than 100 beats per minute.
Strength of the pulse:
- Pulse strength is determined by pulse pressure. Pulse pressure is the difference between the end systolic and end diastolic pressures. E.g. a blood pressure of 120/80 mmHg has a pulse pressure of 40 mmHg (i.e. 120-80=40).
- In atrial fibrillation, pulse strength varies as the random atrial and subsequent ventricular contraction causes an irregularly irregular altered heart rate which means the volume of blood ejected and following pulse pressure vary from beat to beat.
- In ventricular ectopics there is an early beat in the cycle caused by the ventricle spontaneously depolarising. This means that there is a longer pause before the next beat. This means the ventricle has more time to fill and so more blood is pumped out causing a stronger pulse.
Pulse Character/Quality:
- Thready pulse - felt in patients where the end systolic pressure is lower leading to a lower pulse pressure. It is felt as a weak pulse.
- In LV failure the heart cannot beat as strongly so systolic pressure is lower.
- Bounding Pulse - felt in patients where the diastolic pressure is lower. It is felt as a strong pulse.
- Bounding pulse is associated with low peripheral resistance. A dilated vessel gives less resistance to blood flow so diastolic pressure is lower.
- In bradycardia the time between beats is longer allowing more time for diastole so the diastolic pressure drops further widening the pulse pressure.
Raising the arm above the level of the heart drains the venous blood in the arm quicker, lowering the peripheral resistance. This increases the difference between the diastolic and systolic pressures, resulting in an increased pulse pressure. This can be used to exaggerate a bounding pulse.
Locations of Common Pulses
Radial Pulse - felt on the radial side of the wrist.
Brachial Pulse - felt on the medial side of the biceps tendon at the inside of the elbow.
Carotid Pulse - under the jaw anterior to the sternocleidomastoid muscle. Palpate one side at a time only.
Femoral Pulse - felt just inferior to the mid-inguinal point (halfway between ASIS and the pubis).
Popliteal Pulse - felt deep in popliteal fossa (this is a hard pulse to find).
Pedal Pulses:
- Dorsalis Pedis Pulse - lateral to extensor hallucis longus tendon.
- Posterior Tibial Pulse - behind medial malleolus.
The mean arterial pressure can be calculated by either of the following equations:
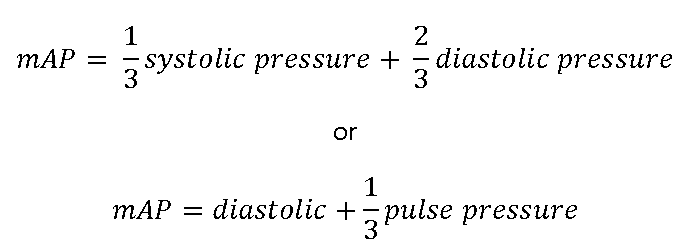
If this falls below around 70 mmHg then organ perfusion can be impaired, depending on the clinical context.
The jugular venous pressure (JVP) is used to measure the pressure in the venous system as the blood is returned to the right atrium. The right JVP is used as it has a straighter course to the right atrium and more reliably reflects right atrial pressure than the left.
This pulse can be seen in the neck when the patient lies at a 45° angle and looks to the left. It should be seen between the two heads of the sternocleidomastoid muscle, just above the clavicle. The JVP is measured as the height of the pulse to the sternal angle. It is measured in cmH2O. It may also be measured using a central line inserted into either the internal jugular vein or superior vena cava and allows a waveform to be measured.
Normally the JVP should not be more than about 3-4 cm above the sternal angle.
Conditions where the JVP can be raised include: right-sided heart failure, cardiac tamponade and volume overload.
- Right-sided heart failure and cardiac tamponade have a raised JVP as the heart is not working as an effective pump. This leads to blood building up in the venous system and raises the venous pressure.
- Volume overload causes an increased volume of blood in the venous system, which raises the venous pressure.
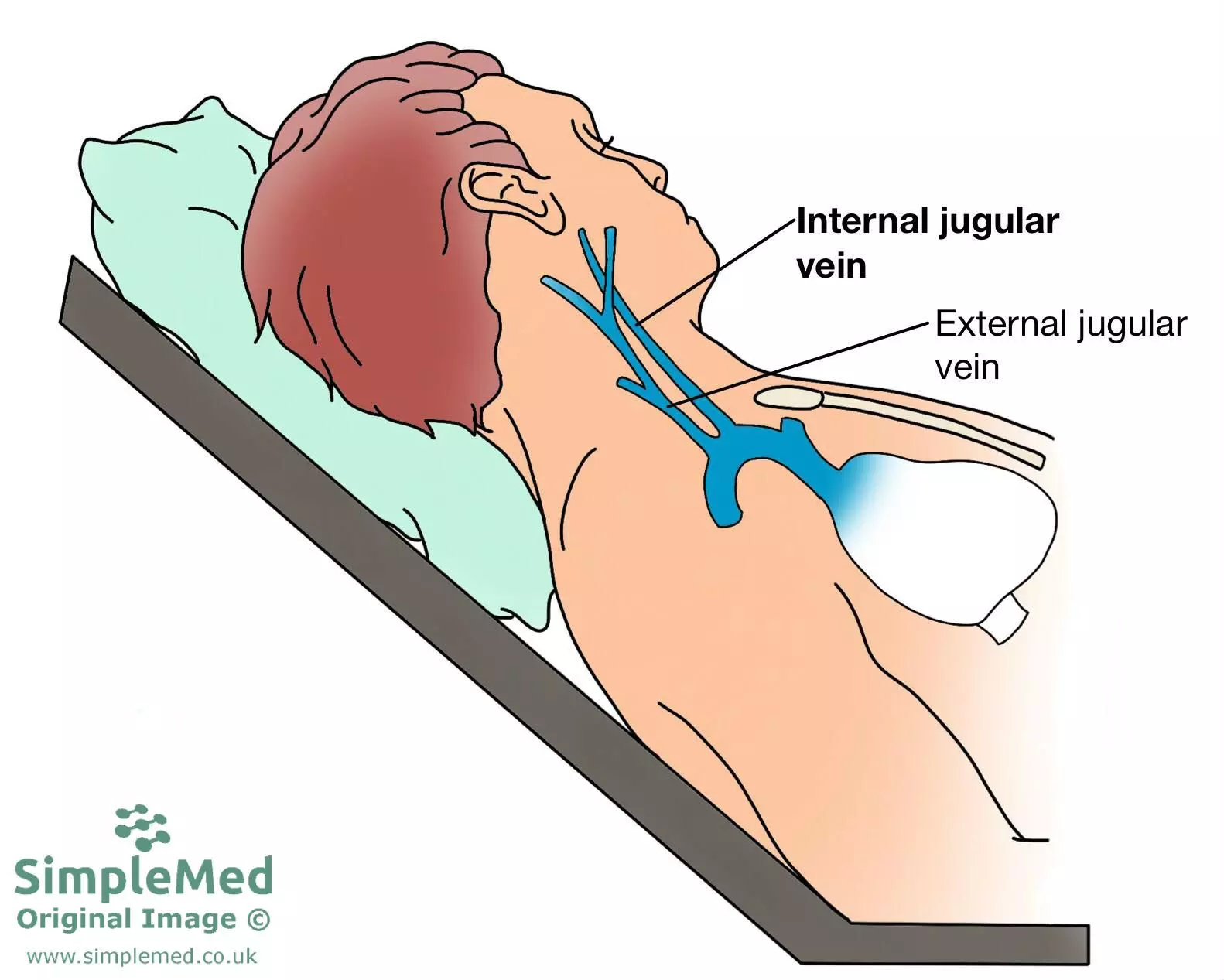
Diagram - The measurement of jugular venous pressure in a clinical setting. Note the 45 degree angle the patient is placed at
SimpleMed original by Dr. Bethany Turner
Reviewed by: Dr. Marcus Judge
- 23799

