Next Lesson - Antibiotics
Abstract
- Sepsis is a life-threatening condition characterised by an unregulated host response to infection, namely, an uncontrolled release of cytokines from the host’s immune response.
- Sepsis Red Flags are key in making the diagnosis of sepsis and should be immediately followed by the application of the Sepsis Six Care Bundle.
- A common cause of sepsis is Neisseria meningitidis. Vaccination against meningitis ACWY is given for prevention.
Core
What is Sepsis? - Identification and Management
Sepsis is life-threatening organ dysfunction caused by a dysregulated host response to infection. It can lead to septic shock (see our article on shock for more detail) - a persisting hypotension (consistently low blood pressure) despite fluid resuscitation which can be rapidly fatal.
In sepsis, damage to the host is mainly caused by the uncontrolled release of cytokines by the host's own immune response which results in circulatory insult and damage to end organs due to ischaemia (lack of blood supply):
Endotoxins on bacteria in the bloodstream trigger a massive (excessive) immune response causing widespread cytokine release. This leads to widespread vasodilation causing an artificially large drop in blood pressure known as distributive shock. This dramatic fall in blood pressure leads to impaired organ perfusion with blood and thus oxygen, followed by dysfunction and death.
This can be further worsened by complications such as DIC (disseminated intravascular coagulation), where multiple clots form within the vessels, using up clotting factors. Cytokines trigger thrombin production, thereby promoting coagulation and also inhibiting fibrinolysis -> the coagulation cascade leads to microvascular thrombosis -> ultimately progressing to organ ischaemia, dysfunction and failure.
Sepsis is a medical emergency and patients can easily and quickly deteriorate.
There are a series of measures which can be used to help identify sepsis early and prevent development of septic shock. These include the EWS (early warning score- standard to all patients) and the SEPSIS RED FLAGS:
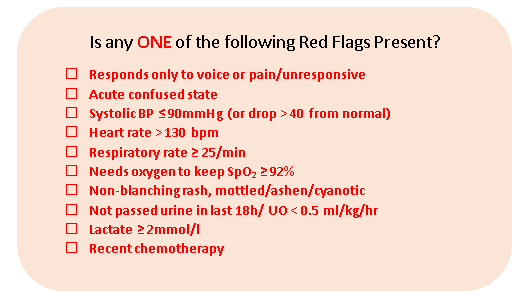
Diagram: The Red Flags for Sepsis. If any of these are present, begin the Sepsis 6 care bundle immediately. It is worth learning these.
SimpleMed original by Dr. Elena Perez
If the patient has an EWS of >3/is visibly unwell, an infection is present or suspected and one of the red flags are true Red Flag sepsis should be suspected and treatment commenced.
The management of sepsis is known as the Sepsis Six Care Bundle:
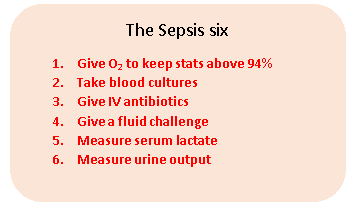
Diagram: The 6 steps that must be taken when a patient is suspected of having Sepsis. A useful mnemonic is BUFALO - Blood Cultures, Urine Output, Fluids, Antibiotics, Lactate, Oxygen.
SimpleMed original by Dr. Elena Perez
The Sepsis six should be carried out in the above order to ensure the most important interventions/ tests are prioritised. The sepsis six can also be remembered as "give 3, take 3".
- Give O2 to titrate oxygen saturation to above 94% (use lower target ranges in patients at risk of hypercapnic respiratory failure, in line with local guidance)
- Take urgent blood cultures- to aid diagnosis
- Give IV antibiotics - (please check with your local antibiotics guidelines)
- Give fluids
- Take serum lactate measurements
- Take a reading of urine output
Details of each step and the pathway for diagnosis are outlined on the Sepsis 6 form used when administering treatment. Some further investigations that may be useful include; full blood count, urea and electrolytes, blood sugar, Liver Function Tests (LFTs), C-Reactive Protein (CRP, a marker for inflammation), Arterial Blood Gas (ABGs), coagulation studies and further microbiology samples (CSF, urine, organism specific blood PCR, etc.). These will allow more precise identification of the causative organism and provide more information for specific antibiotic treatment. However, these investigations take time and empirical IV antibiotics should be given prior to full identification of the organism as part of the Sepsis 6 bundle.
The most likely causative organism varies by the age of the patient and guides antibiotic treatment.
The example of Neisseria meningitidis
A common cause of sepsis is Neisseria meningitidis. It is a gram-negative bacterium, often found as a diplococcus and part of the normal flora in the nasopharynx of about 10% of the population. However, if it enters the blood stream and reaches the brain it may cause meningococcal meningitis, with the potential to escalate into meningococcal sepsis. There are different serogroups of N. meningitidis classified based on their polysaccharide capsular antigen (one of its main virulence factors that confers it varying pathogenicity). Current vaccination covers the serogroups ACWY, and a serogroup B vaccine is also included in the routine UK childhood immunisation programme.
Prevention consists of vaccination and antibiotic prophylaxis to recent contacts of the patient.
The classic symptoms of meningococcal meningitis are a non-blanching purpuric rash (tested using the glass or tumbler test), a stiff neck, confusion, dislike of bright lights (photophobia), drowsiness, aching muscles and joints. In neonates, the fontanelle may be bulging and tense. In this case, the empiric choice of antibiotic is ceftriaxone (a cephalosporin) as it has the ability to penetrate into the CSF which is the site of infection of N. meningitidis.
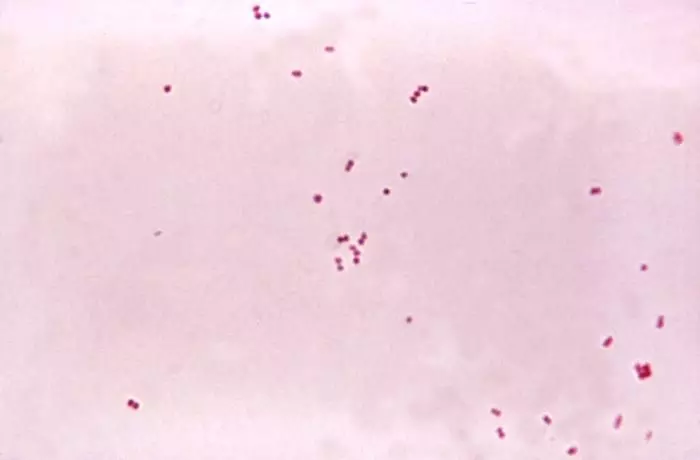
Figure: Gram negative (pink) diplococci (pairs of circular bacteria) - these are most likely N. meningitidis, the main cause of meningococcal meningitis
Public Domain Image - Dr. Brodsky [Public domain]
For other cases of sepsis without signs of meningitis, empiric antibiotic treatment should follow local NHS trust guidelines and usually involves a broad-spectrum beta-lactam tailored to the suspected source of infection. Aminoglycosides such as gentamicin may be added in selected cases but are not used as sole first-line therapy. Reserve agents such as meropenem are typically used only when indicated by local policy or microbiology advice. When in doubt, the trust you are working under (if you are working within the NHS) will have guidelines of first and second line treatments for a wide range of conditions, including sepsis.
Editor’s note: It is highly recommended to visit sepsistrust.org for up to date resources and information to complement this article. Sepsis is a cornerstone of medical management and risk.
Edited By: Dr. Marcus Judge and Dr. Ben Appleby
- 15279

