Next Lesson - The Lymphatic System
Abstract
- Regeneration is the replacement of damaged tissue, and the end result is as if no damage occurred.
- Organisation of tissues will result in scarring and can occur by primary intention in clean, non-infected wounds with opposed edges, or secondary intention where there has been more tissue loss.
- Organisation requires several processes including:
- Haemostasis to deliver the required components.
- Inflammation due to the tissue injury.
- Regeneration of structures that have been destroyed.
- Scarring.
This article will explain how tissue regeneration and repair occurs, and some defects that may affect it.
Core
Regeneration allows replacement of damaged tissue through cell replication and growth of tissues. The end result of regeneration may not fully restore the original function or structure, and the tissue may exhibit differences compared to the original. Tissues can regenerate completely after injury if there is:
- An intact connective tissue scaffold
- A population of stem cells
If the injury is too extensive, or the harmful cause persists then regeneration will not be able to occur. This will result in formation of a scar after the process of organisation - healing by primary or secondary intention.
The ability of a tissue to regenerate depends on the stem cell population, which are cells that can differentiate and replace cells that have been lost to injury or normal senescence. They are present in small, discrete populations. For example, in the basal layer of epidermis, or at the bottom of intestinal crypts.

Diagram - The bottom of intestinal crypts where stem cells are found. The stem cells can divide and differentiate to replace lost cells of the intestinal epithelium.
Creative commons source by STEMCELL Technologies Inc [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
When stem cells undergo mitosis, one of the daughter cells remains as a stem cell and the other differentiates to become a mature cell to meet the needs of the tissue it is in. This is asymmetric replication.
Stem cells can be classified according to how many types of other cells they can differentiate into.
- Unipotent
- Only able to differentiate into one type of cell.
- For example, stem cells in the basal layer of the epidermis.
- Multipotent
- Able to produce several types of differentiated cells.
- For example, haematopoietic stem cells in bone marrow.
- Totipotent
- Able to differentiate into any type of cell.
- For example, the zygote and early embryonic cells.
Cells can be organised into 3 different groups depending on their proliferative activity. These are:
- Labile
- These cells are short lived, and can easily be replaced by replication and maturation of stem cells.
- This means these tissues have a high reproductive capacity.
- For example, epithelial cells (such as those in the gastrointestinal tract).
- Stable
- These cells normally have a slow rate of cell replication.
- However, they can divide rapidly when required.
- Hepatocytes and renal tubular cells are examples of stable cells.
- Permanent
- These cells are unable to undergo effective replication.
- Only a few stem cells are present.
- Neurones are an example of permanent cells.
Regeneration can take place in tissues with labile and stable tissues when tissue damage isn’t extensive. The presence of stem cells makes this possible, as they can divide and differentiate to replace the lost cells.
Cell to cell communication occurs via local mediators such as growth factors, hormones or by direct cell-cell or cell-stroma contact. This communication allows control of regeneration.
Local Mediators
Growth factors are a type of local mediator, and are important in regeneration and fibrous repair. Growth factors are polypeptides. Many growth factors, or their receptors, are encoded by proto-oncogenes. They act in an autocrine (acting on the cell itself that secretes the growth factor) or paracrine (acting on cells a short distance away) manner. They stimulate or inhibit cell proliferation through binding to specific receptors to stimulate gene transcription.
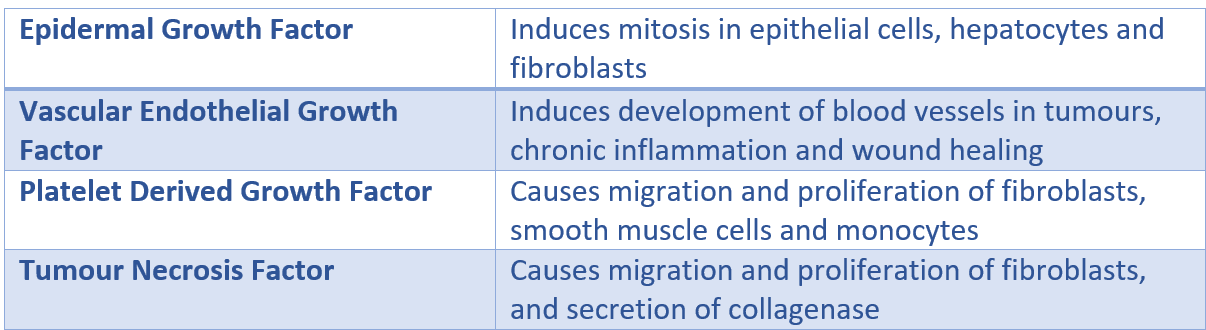
Table - shows some of the different growth factors in the body and their effect
SimpleMed original by Dr. Emily Smith
Contact Inhibition
Cells will continue to replicate until they are in contact with other cells, which triggers a signal to stop proliferation, a process known as contact inhibition. This ensures that there is no overlap of cells. There are proteins called adhesion molecules which bind cells to each other (cadherins) or to extracellular matrix (integrins).
Whilst regeneration involves the growth of a tissue back to its normal state, organisation is the process by which specialised tissues that have suffered damage undergo fibrous repair to form a scar. It requires collagen which is synthesised by fibroblasts and myofibroblasts. Depending on the extent of the tissue damage, organisation can take place by either primary or secondary intention, but the general process remains the same:
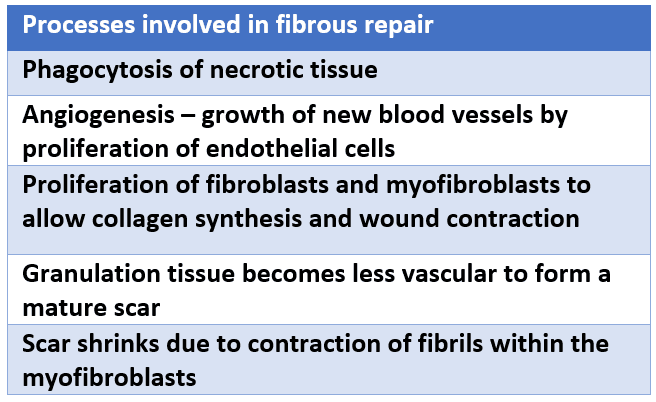
Table - The processes in fibrous repair from initial injury to the formation of a scar.
SimpleMed original by Dr. Emily Smith
The formation of granulation tissue is part of the process of organisation. Granulation tissue fills in the gap that is initially left by the damage to tissue. Angiogenesis (formation of new blood vessels) occurs within the granulation tissue, and the new capillaries provide oxygen, nutrients and cells required to repair the damage.
Granulation Tissue Cells
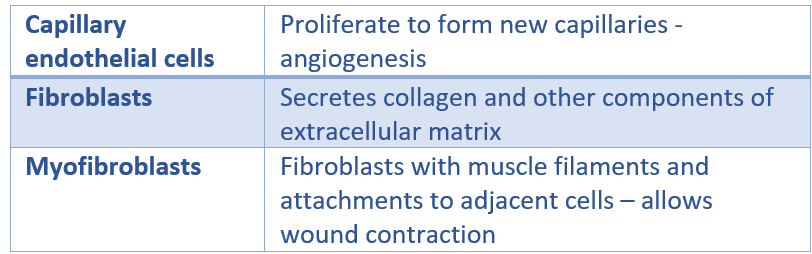
Table - The different cells found in granulation tissue
SimpleMed original by Dr. Emily Smith
Histology of granulation tissue can be seen in the image below:

Image - The histology of granulation tissue in an infected wound. There are many blood vessels and immune cells.
Creative commons source by Patho [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
This can occur in clean, non-infected wounds with opposed edges. These wounds result in the death of a limited number of epithelial and connective tissue cells, and the disruption to the basement membrane.
- Haemostasis - occurs within seconds to minutes. Severed arteries contract, and the space fills with blood. A scab forms which seals off the wound from the outside world to prevent entry of bacteria.
- Inflammation - occurs within minutes to hours. Neutrophils appear at the edges of the wound.
- Migration of cells - occurs after 48 hours. Macrophages phagocytose dead neutrophils and secrete cytokines. These cytokines attract fibroblasts and endothelial cells. Spurs of endothelial cells are also present, these deposit components of basement membrane.
- Regeneration - occurs around day three. Granulation tissue invades the space. There is also proliferation of epithelial cells to thicken the epidermis, which leads to the scab falling off. Angiogenesis continues.
- Early scarring - occurs within 7-10 days. Fibroblasts in the granulation tissue proliferate and deposit collagen fibres to form a scar.
- Scar maturation - the scar is now a mass of fibrous tissue with collagen fibres, few cells and few vessels. Capillaries disappear over time, which means old scars may appear white, although this can vary based on factors such as the depth of the wound, infection, and individual healing responses.
Healing by Secondary Intention
This occurs in wounds with tissue loss, separated edges or infected wounds. The wounds are filled by abundant granulation tissue which forms the margins of the wound. The same processes occur as in healing by primary intention, however, there is a more intense inflammatory process, and considerable wound contraction. The wound contracts towards the centre which means that the final scar takes on the shape of the original wound.

Diagram - The process of healing by primary and secondary intention and how the processes differ from each other
SimpleMed original by Dr. Emily Smith
Factors Affecting Regeneration and Repair
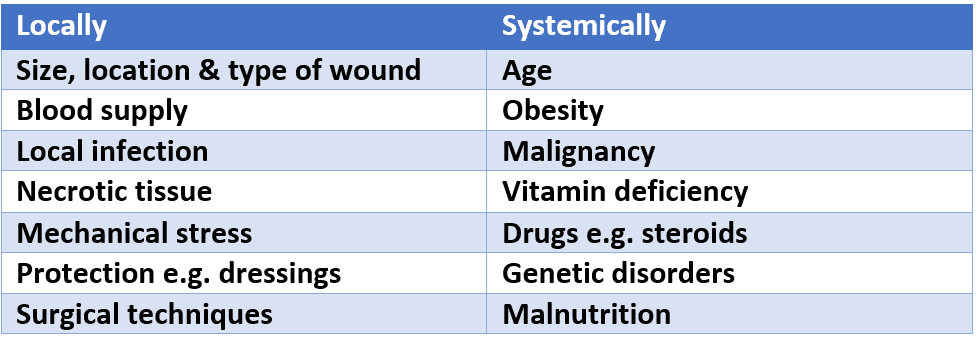
Table - The factors affecting regeneration and repair
SimpleMed original by Dr. Emily Smith
Scurvy:
- Caused by a Vitamin C deficiency, which is required for hydroxylation of procollagen.
- Scurvy causes people to be unable to heal wounds, and they tend to bleed due to fragile capillaries.
- Also, because the collagen in scars is constantly being turned over, people who develop scurvy are at risk of old scars reopening due to the inability to replace the collagen.
Ehlers-Danlos Syndrome:
- This is an inherited syndrome which causes collagen fibres to lack tensile strength.
- People with this have hyperextensible and fragile skin, and hypermobile joints.
- They also suffer from poor wound healing and are predisposed to joint dislocation.
- In some subtypes, particularly the vascular type, this condition can cause rupture of the colon or large arteries.
Complications of Fibrous Repair
Insufficient fibrosis:
- This can result in hernias or ulceration.
Formation of adhesions (fibrous bands between or around structures):
- Can compromise organ function, potentially leading to complications such as bowel obstruction.
Loss of function:
- Due to replacement of specialised parenchymal cells by scar tissue.
- For example, scar tissue formed after a myocardial infarction can’t contract with myocytes.
Excess scar contraction
- Can cause obstruction of structures, including blood vessels which can lead to its own complications.
Overproduction of collagen:
- Results in a keloid scar.
- Keloid scars don’t regress, and they exceed the margins of the scar.
- Excision of a keloid scar is associated with a high risk of recurrence, particularly if performed without adjuvant therapy.

Image - A Keloid scar
Creative commons source by Micheal Rodger [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Edited by: Dr. Bethany Turner
Reviewed by: Dr. Thomas Burnell
- 18875

