Next Lesson - Conditions of the Hand
Core
Want more information on anatomy before you begin looking at conditions? Head to our articles on Bones of the Hand, Muscles of the Forearm and Bones of the Upper Limb for more information!
Scaphoid fractures account for 70-80% of all carpal bone fractures. They are caused by a fall onto an outstretched hand (FOOSH) and are most common in young adults.
A scaphoid fracture presents with pain in the anatomical snuffbox (a region just below the base of the thumb) that is exacerbated by movement. Complications include a high risk of non-union and avascular necrosis due to the scaphoid bone having a retrograde blood supply (meaning if there is a fracture that disrupts blood supply, the bone may not heal).
The fracture may not show on the initial X-Ray, but the patient should be treated as if a fracture is present. Then a repeat X-ray may be done 10-14 days later, as the fracture can become visible due to bone resorption along the fracture line, although early MRI or CT is often used to confirm the diagnosis. Treatment may or may not require surgery but a splint or cast is used to increase chances of union of the bone fragments.
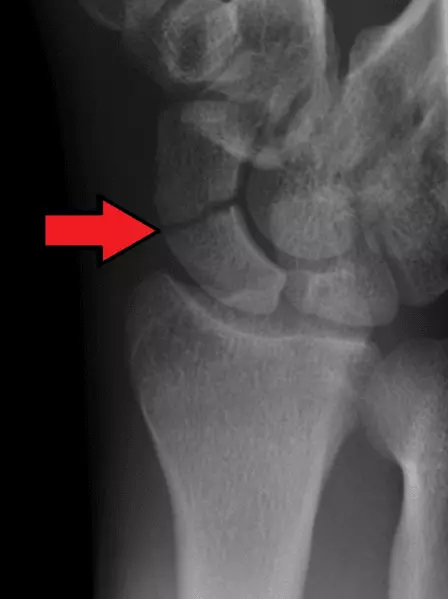
Image - An X-Ray showing a scaphoid fracture. The red arrow shows the fracture line
Creative commons source by Gilo1969 [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
A Colles’ fracture is an extra-articular fracture of the distal radius with dorsal angulation and impaction (meaning if the fracture looked like this >, the larger end would be on the dorsal side). It is caused by a FOOSH, with a pronated forearm and dorsiflexed wrist.
This condition presents with pain, a 'dinner fork' deformity and swelling. An associated ulnar styloid process fracture is relatively common. Treatment may include casting or surgery.
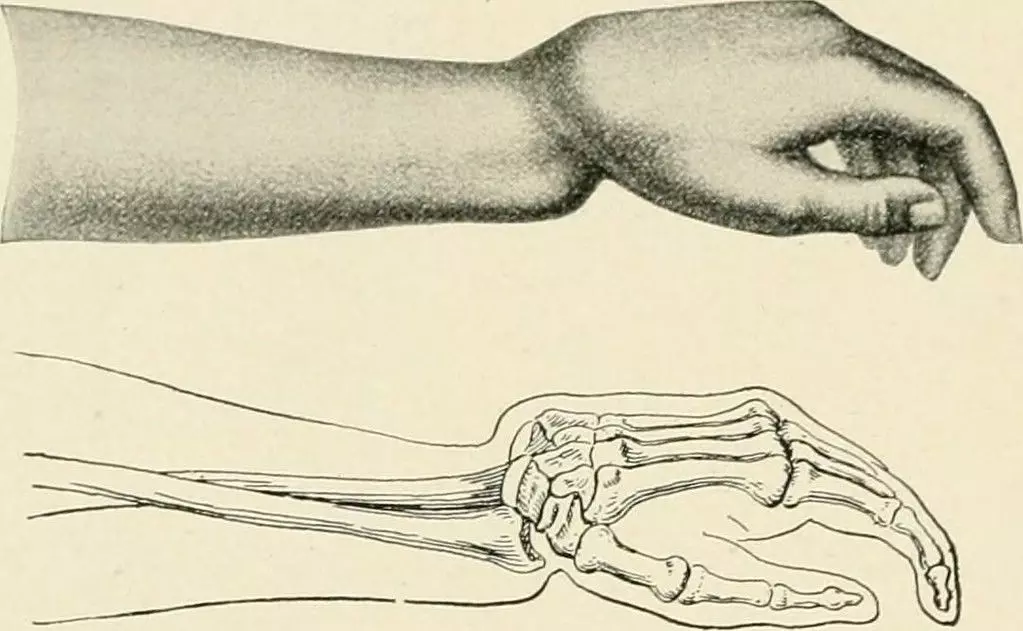
Image - A drawing of a Colles' fracture
Creative commons source by The Practice of Surgery by Mumford, James Gregory (1910) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
A Smiths’ fracture is an extra-articular fracture of the distal radius with volar/palmar angulation and impaction (meaning the open bit of the > shaped fracture is on the palmar side). It is caused by a fall onto a flexed wrist or a blow to the back of the wrist. This condition is relatively rare but usually occurs in young males or elderly females.
It presents with pain, a 'garden spade' deformity and swelling. Complications include malunion leading to permanent garden spade deformity, which can in turn lead to carpal tunnel syndrome. Treatment may include casting, closed reduction or surgery.
Carpal tunnel syndrome is the compression of the median nerve as it passes through the carpal tunnel from the forearm into the hand. Risk factors for this condition include: being female, obesity, pregnancy, rheumatoid arthritis and hypothyroidism. It can also present in those who frequently rest on the palmar side of the wrist e.g. when typing. It presents with paraesthesia in the palmar aspect of digits 1-3 and the lateral half of the 4th digit. There is weakness of abduction and opposition of the 1st digit.
Sensation to the palm is spared as the palmar cutaneous branch of the median nerve does not enter the carpal tunnel. Adduction of the 1st digit is typically spared as it is supplied by the ulnar nerve, whereas weakness mainly affects abduction and opposition of the thumb.
Non-surgical treatment includes bracing or splinting and NSAIDs to reduce inflammation and manage pain, as well as avoiding or modifying harmful activities. If the symptoms are more severe, however, surgery followed by exercises to regain full movement is the usual treatment plan.
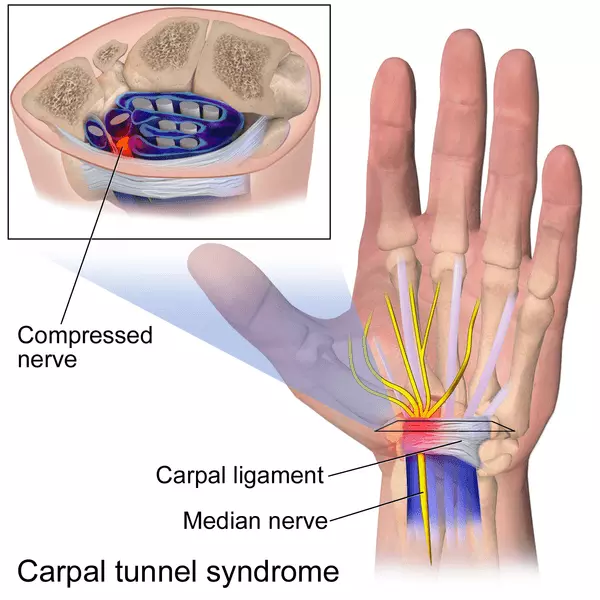
Diagram - The location where the median nerve is compressed in carpal tunnel syndrome
Creative commons source by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Ulnar Nerve Compression in Guyon’s Canal
Ulnar nerve compression in Guyon’s canal is also known as ‘Handlebar palsy’ and is caused by entrapment of the ulnar nerve as it passes superficial to the flexor retinaculum through a tunnel between the pisiform and the hook of hamate. This condition is relatively common in cyclists, hence the name ‘Handlebar palsy’.
It presents with paraesthesia and weakness of flexion/extension of the 4th and 5th digits. There is also weakness of adduction of the 1st digit.
Initial treatment is anti-inflammatory drugs or corticosteroid injections. If this is unsuccessful, surgery is used to reduce the compression on the ulnar nerve by relieving the tension on the volar carpal ligament (which forms the roof of Guyon’s canal).
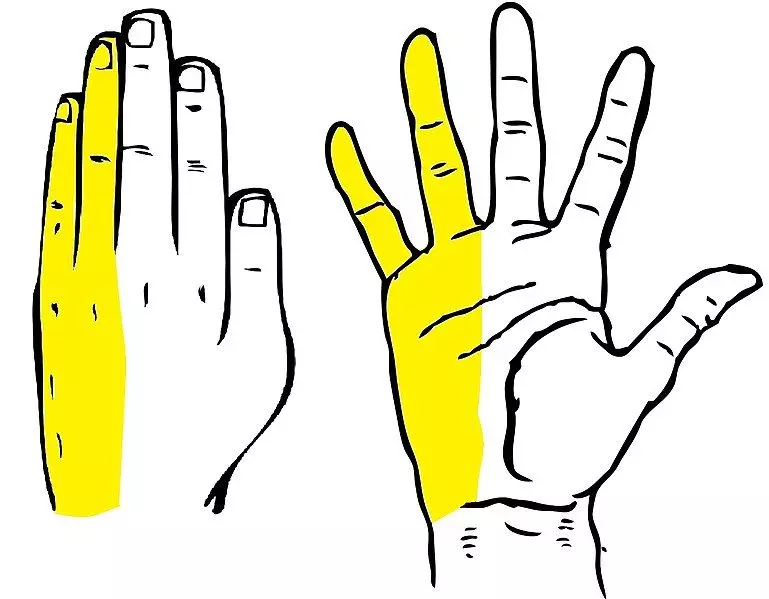
Diagram - The sensory distribution of the ulnar nerve in the hand
Creative commons source by Clker Free Vector Images [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
A low injury to the median nerve occurs due to a penetrating injury to the wrist. It presents with an ‘Ape hand deformity’ - flattened thenar eminence and an adducted/externally rotated 1st digit due to paralysis of lumbricals and thenar muscles.
Sensation to the palm remains intact as the palmar cutaneous branch is usually spared.
Treatment ranges from rest and avoiding aggravating activities to surgery as the severity increases. Treatment can also include corticosteroid injections, splinting and physical therapy.

Image - A hand with ape hand deformity
Creative commons source by Emily Barrett [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
A low injury to the ulnar nerve occurs due to a penetrating injury at the wrist. It presents with a ‘low ulnar claw’ - hyperextension at the metacarpophalangeal joints, and flexion at the interphalangeal joints of the 4th and 5th digits. There is also paraesthesia of the palmar aspects and the distal dorsal aspects of the 4th and 5th digits.
The sensation of the ulnar border of the hand will be spared.
Treatment ranges from rest and avoiding aggravating activities to surgery as the severity increases. Treatment can also include corticosteroid injections, splinting and physical therapy.
It is important to differentiate this from the appearance of the hand in a high ulnar nerve injury, shown in the article Conditions of the Arm. Unexpectedly, the appearance of the low ulnar claw is more severe than the appearance of the high ulnar claw. This is because with a high ulnar nerve injury, the innervation to flexor digitorum profundus is destroyed, meaning the fingers cannot flex as much as they can in a low ulnar nerve injury, when this muscle is spared. This is called the ‘Ulnar paradox’.

Image - A hand with a low ulnar claw deformity
Creative commons source by Mcstrother [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Reviewed by: Dr. Thomas Burnell
Edited by: Dr. Maddie Swannack
- 6695

