Next Lesson - Protein and Amino Acid Metabolism
Abstract
- Lipids are a key energy storage molecule in the body and can be metabolised to release energy.
- Examples of important lipids in the body include phospholipids, lipoproteins, cholesterol, and apolipoproteins.
- Ketone bodies are produced to be used as an energy source during times of low glucose.
- Lipoproteins allow the movement of lipids around the body so that they can be used for processes such as the production of steroid hormones or bile salts.
- There are three main diseases in this article relating to the metabolism of lipids which are hyperlipoproteinaemia, hypercholesterolaemia and atherosclerosis. These diseases can be serious and are all related to elevated lipid levels. Lifestyle improvements such as a healthy diet and exercise are key to management along with medications such as statins.
Core
Lipids are a structurally diverse group of molecules which are hydrophobic and contain carbon, hydrogen and oxygen.
There are 3 classes of lipid:
- Fatty acid derivatives - fatty acids, triacylglycerol and phospholipids
- Hydroxy-methyl-glutamic acid derivatives - ketone bodies and cholesterol
- Vitamins - fat-soluble vitamins A, D, E and K
The main storage form of lipid in the body is in the adipose tissue. Adipose stores energy in the form of triacylglycerol (TAG, also known as triglycerides), a structure made up of one hydrophilic molecule of glycerol attached to three hydrophobic fatty acid chains.
As lipids are hydrophobic, it is not feasible to transport them freely in the blood. This means that free fatty acids are transported attached to albumin, and TAGs being produced in the liver are transported in lipoproteins. This allows the TAGs to be targeted to the peripheral tissues that need them. Lipid transport is explained later in more detail.
- Phospholipids - two non-polar fatty acid chains bound to glycerol with a phosphate group (it is very similar in structure to a TAG, but with a phosphate group replacing one of the fatty acids). They form bilayers (used to form cell membranes), micelles, and liposomes.
- Cholesterol - synthesised in the liver. Cholesterol is a precursor to steroid hormones and bile acids.
- Lipoproteins - a sphere of phospholipids used to transport lipid in the bloodstream. They can have proteins attached on the outside or in the centre, called apolipoproteins. There are five types of lipoprotein, with different functions, as shown in the table below.
- Apolipoproteins - the peripheral and integral proteins on lipoproteins. They can have structural (packaging) or functional (co-factors and ligands) roles.
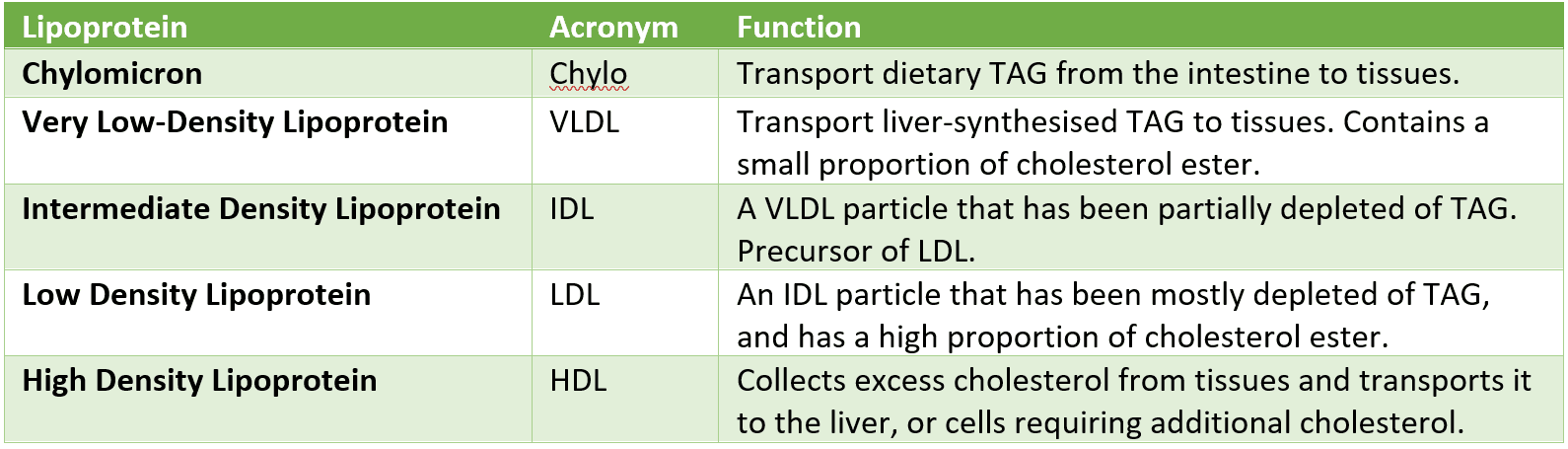
Table - The different types of lipoproteins found in the body
SimpleMed original by Dr. Maddie Swannack
Fatty acids have the general structure of CH3(CH2)nCOOH. The carbon chain is commonly between 14 and 18 carbons long, and can have many variable features, such as being saturated or unsaturated, or amphipathic (a mix of hydrophobic and hydrophilic parts). Fatty acids are transported into the mitochondria through the carnitine shuttle, a system that allows long-chain fatty acyl groups to cross the double membrane of the mitochondria. This involves transfer of the fatty acyl group between CoA and carnitine (an ammonium compound), allowing it to be carried across the two membranes.
Once inside the mitochondria, the fatty acid is catabolised through a process called beta oxidation. With each cycle of beta oxidation, a two-carbon molecule is liberated from the fatty acid (making the fatty acid 2C shorter each time until it has been fully degraded). This molecule goes on to become acetyl CoA, which is used in the Krebs Cycle to generate energy.
During the process of beta oxidation, NADH and FADH2 are made which can be used to produce energy in the electron transport chain.
Fatty acids are more reduced than carbohydrates, meaning fatty acids release more molecules of ATP per carbon during respiration than carbohydrates.
While long-chain fatty acids are not used by the brain because they do not effectively cross the blood-brain barrier, the brain can utilise ketone bodies as an energy source during periods of low glucose availability. Additionally, lipid metabolism does not occur in red blood cells (because they have no mitochondria).
Glycerol is a component of TAGs. This diagram shows how NADH is produced from glycerol to be used for ATP production in the electron transport chain. The metabolites of glycerol are used to produce intermediates for use in glycolysis and triacylglycerol synthesis.
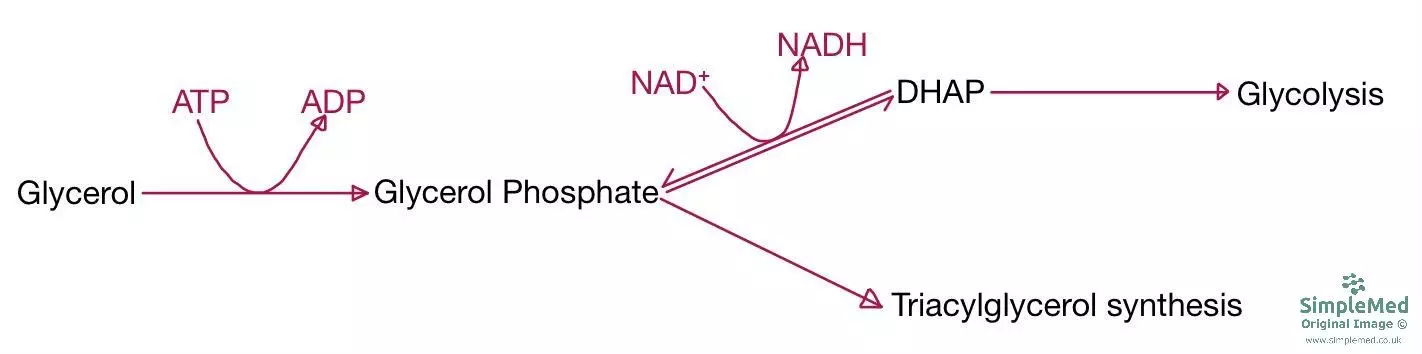
Diagram - The metabolic pathway of glycerol to be used in glycolysis
SimpleMed original by Dr. Maddie Swannack
Ketone bodies are water soluble molecules produced by the liver. There are three types: acetoacetate, beta-hydroxybutyrate, and acetone.
They can act as an alternative substrate in starvation (physiological ketosis) or untreated type 1 diabetes mellitus (pathological ketosis). In starvation, glucose availability is reduced, and as lipids cannot cross the blood-brain barrier, ketone bodies are required as they can cross the blood-brain barrier. The brain can use these as an energy source when glucose is in short supply.
Lipids eaten in the diet are hydrolysed in the small intestine by pancreatic lipases and then transported across the brush border into the lacteals (lymphatic vessels which transport digested fat, all other substances are transported in the blood). Lipids are transported in chylomicrons as TAGs and can be stored in adipose tissue if there is plenty of glucose (i.e. they are not needed as a fuel source immediately).
This diagram shows the fatty acid cycle as it occurs in adipose tissue. It illustrates how, with a constant supply of glucose, the stored fatty acids are not static (they are continually cycling).
However, if the supply of glucose is too low, reaction 3 cannot take place (because there is insufficient glycerol-3-phosphate available), so the fatty acids and glycerol exit the cycle and are released into the blood to be used as an alternative fuel source.
This release of fatty acids and glycerol is under hormonal control triggered by glucagon (released when glucose levels are low), which activates the hormone-sensitive lipases to break down the triglyceride to provide an alternative fuel source.
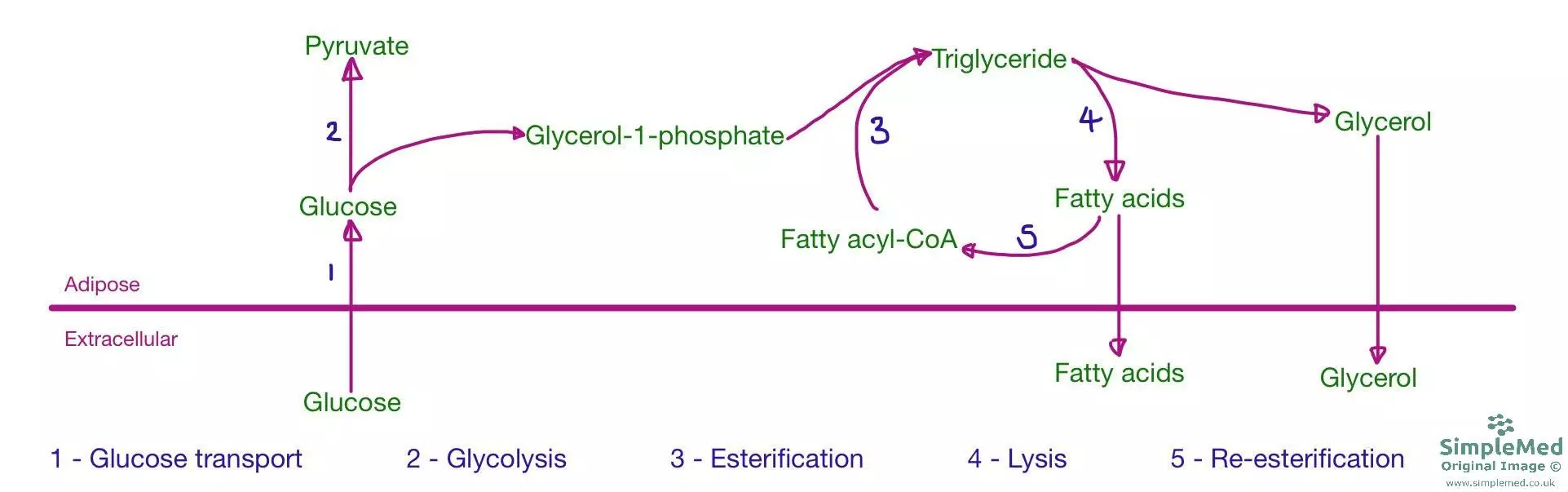
Diagram - The metabolic pathway of the storage of TAGs in adipose tissue. Glucose is taken up by adipocytes and turned into triglycerides, which can be released as fatty acids and glycerol when blood glucose is low
SimpleMed original by Dr. Maddie Swannack
This diagram shows the formation and metabolism of chylomicrons. Lipid moves from the small intestine to the lymph via lacteals in the villi, and then is emptied into the blood via the thoracic duct into the left subclavian vein. At the walls of capillaries, chylomicrons are partially metabolised by lipoprotein lipase, supplying lipid to cells that need it. Once the lipid content of the chylomicron falls below 20%, it becomes a chylomicron remnant, and travels to the liver to finish being broken down.
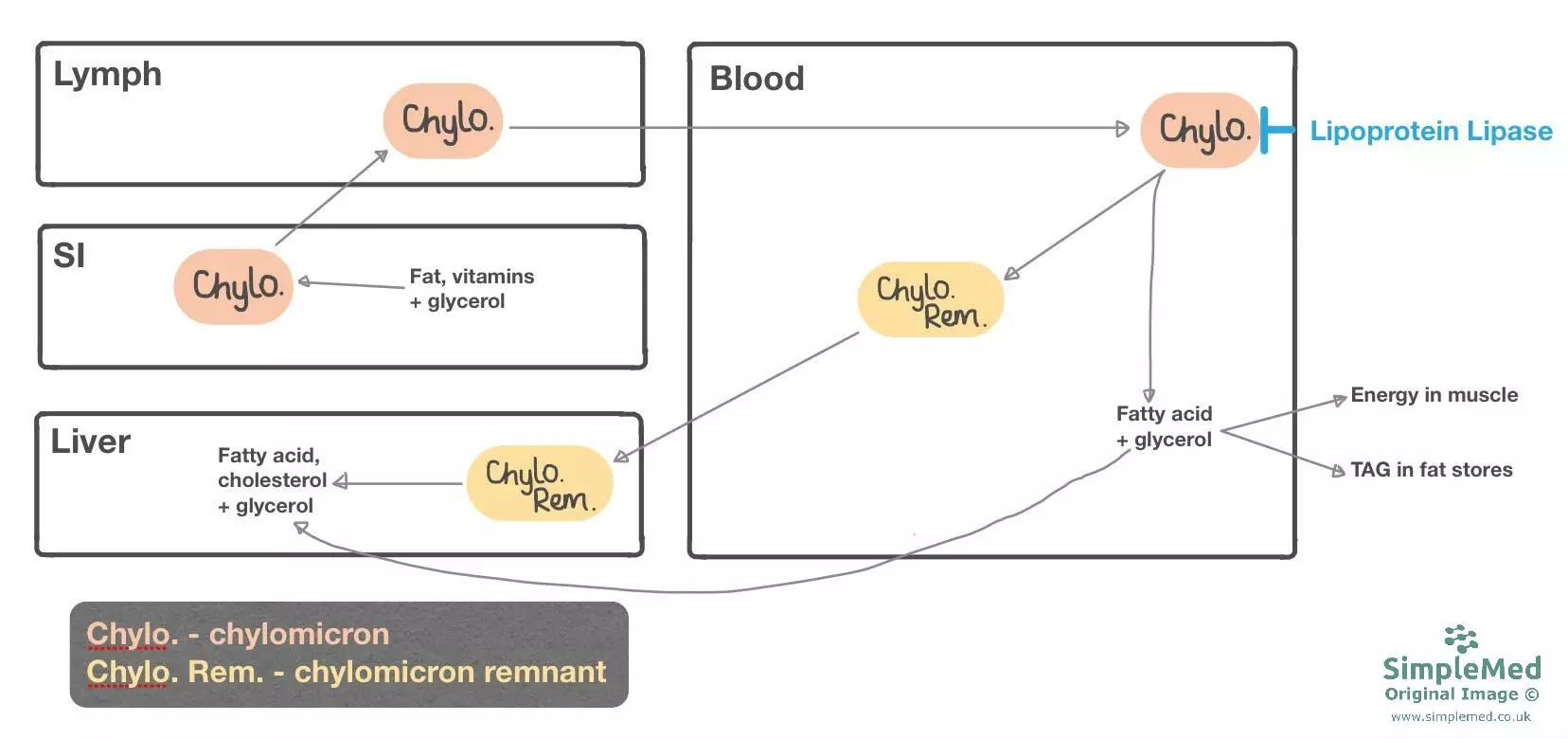
Diagram - The pathway of chylomicrons from the small intestine, to the lymph, to the blood in order to release fatty acids and glycerol to tissues. When the chylomicron becomes depleted, it becomes a remnant and travels to the liver for metabolism
SimpleMed original by Dr. Maddie Swannack
This diagram shows how cholesterol and TAG produced in the liver travel around the body to supply muscles and fat stores.
The triglycerides are released by the liver contained within a Very Low-Density Lipoprotein (VLDL), which contains predominately lipid, and a small proportion of cholesterol ester. As the lipoprotein is metabolised by lipoprotein lipase, its TAG content is depleted, and the particle becomes an Intermediate Density Lipoprotein (IDL). Once the TAGs have been almost completely removed, and the predominant molecule is cholesterol ester, the lipoprotein is now called a Low-Density Lipoprotein (LDL).
LDL enters hepatocytes or cells that need cholesterol and express receptors for the ApoB-100 ligand on the LDL. The LDL gets taken into the cell by endocytosis, and then is digested by lysosomes.
LDL is often referred to as 'bad cholesterol'. This is because it has a long half-life, meaning it may be present in the blood long enough to become oxidised. This involves being phagocytosed by macrophages to form foam cells and can contribute to atherosclerosis. This is the reason that having a low level of LDL cholesterol is good, because it means that the risk of forming these foam cells is reduced, so the risk of atherosclerosis is reduced.
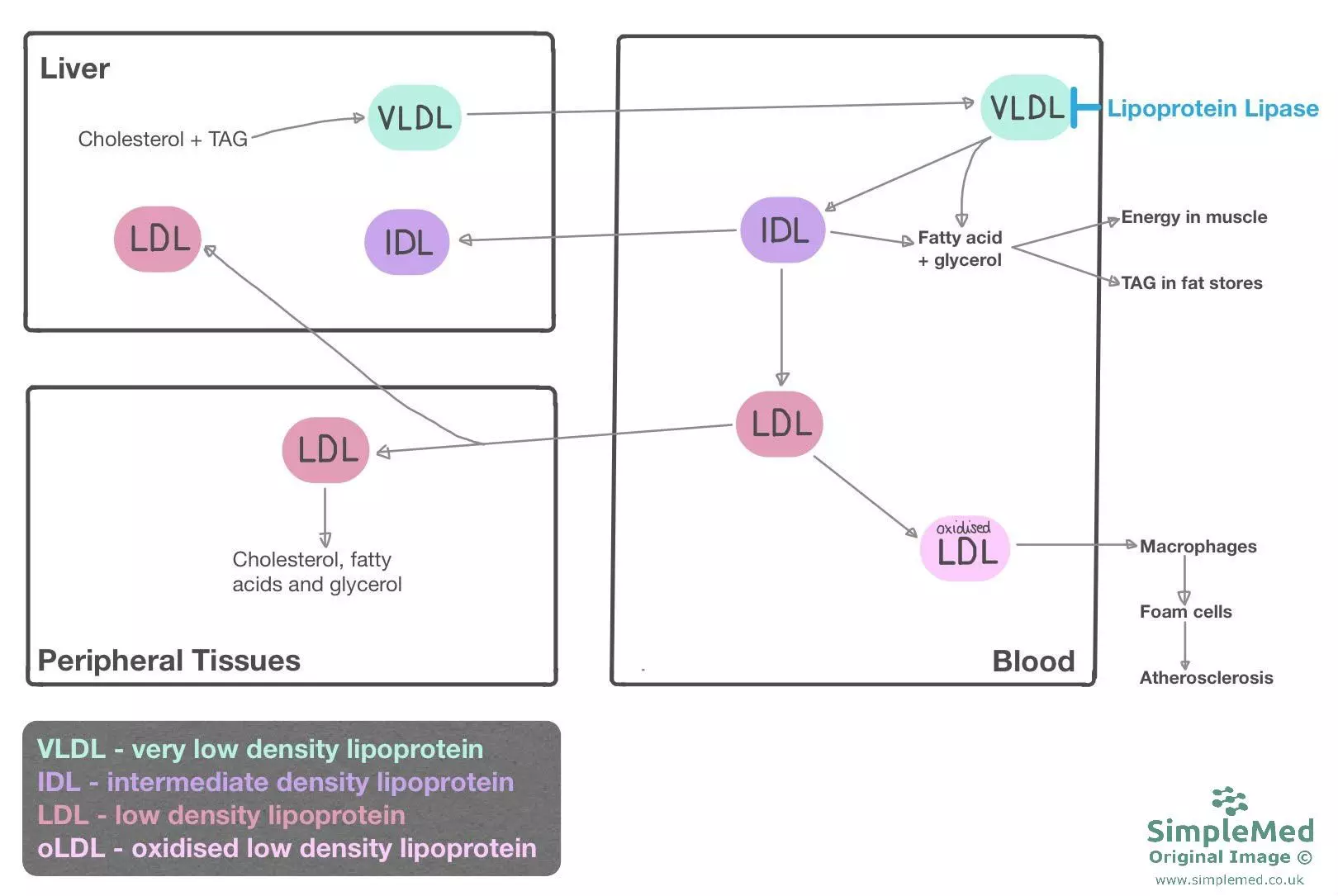
Diagram - The pathway of lipoproteins in the body. Lipoproteins deliver TAGs to peripheral tissues using the enzyme lipoprotein lipase. The diagram also shows how LDL can become oxidised and contribute to the formation of atherosclerotic plaques
SimpleMed original by Dr. Maddie Swannack
This diagram shows how an empty HDL particle is released from the liver and intestine and receives excess cholesterol from body cells and LDL. It then transports this to the liver or steroidogenic cells. This means it can be used to produce steroid hormones and bile salts. HDL is also known as 'good cholesterol' as it removes excess cholesterol from peripheral tissues, reducing the chance of atherosclerosis.
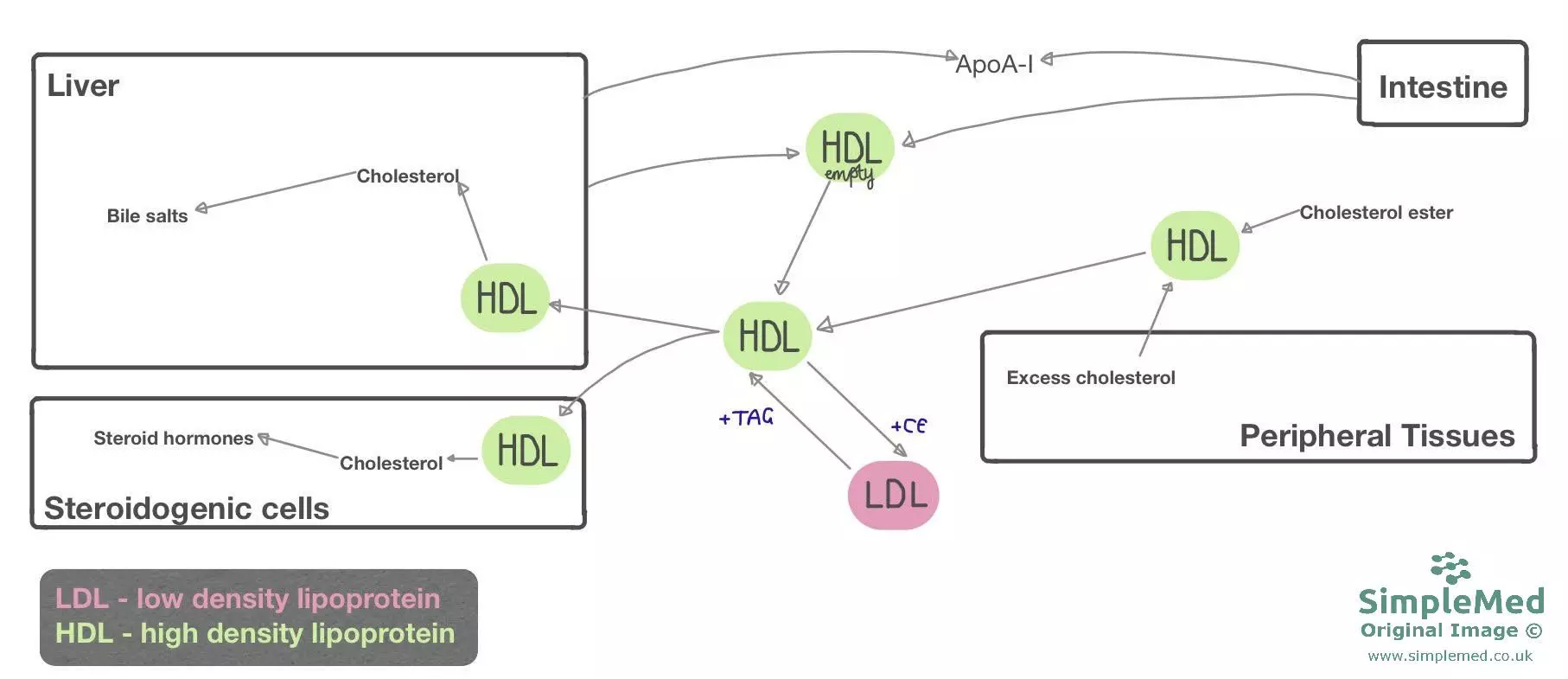
Diagram - The pathway of HDL particles through the body to collect excess cholesterol from body cells and LDL particles, and deliver cholesterol to cells that need it
SimpleMed original by Dr. Maddie Swannack
Included here are three diseases relating to lipid metabolism. This is not an exhaustive list, but they act as examples of how impaired lipid metabolism can lead to pathology . For more information see the article on Atherosclerosis.
Hyperlipoproteinaemias are a group of diseases that present with high levels of one or more class of lipoprotein caused by overproduction or under-removal. There are six types and each one has a different defective component. Here are three examples:
- I - chylomicrons present in the plasma even when fasting due to a defective lipoprotein lipase.
- IIa - a defective LDL receptor leading to high levels of LDL in the blood. This condition predisposes to atherosclerosis due to oxidised LDL levels being high.
- III - raised IDL and chylomicron remnants due to a defective ApoE (lipoprotein) on the surface preventing the lipoproteins to be metabolised.
Treatments for hyperlipoproteinaemias include improving diet, increasing exercise, statins (inhibiting an enzyme used in cholesterol production called HMG CoA reductase, to reduce the amount of cholesterol synthesised), and bile salt sequestrants (keeps bile salts in the intestine leading the liver to increase production and thus use up excess cholesterol in the blood to make more).
Hypercholesterolaemia patients present with very high levels of cholesterol in the blood, which can manifest characteristic external signs such as xanthelasma (yellow patches on the eyelid), tendon xanthoma (nodules on tendons), and corneal arcus (a white line around the iris). These signs are due to the deposition of cholesterol in tissues.
Treatments for hypercholesterolaemias are similar to the treatments for hyperlipoproteinaemias: diet, exercise, statins and bile salt sequestrants.
Raised serum LDL is associated with the formation of atherosclerotic plaques. This happens due to the longer half-life of LDL, giving LDL a higher chance to become oxidised and phagocytosed by macrophages to form foam cells. This can lead to the narrowing of arteries, which can cause angina, and the formation of atherosclerosis can increase the chances of thrombus formation, leading to an MI or a stroke.
- Total cholesterol < 5 mmol/l
- Total cholesterol: HDL ratio = lower is better (for example, 4 is better than 6).
- Total lipid values are not routinely used in clinical practice and are less helpful than individual lipid measurements.
Edited by: Dr. Ben Appleby and Dr. Bethany Turner
Reviewed by: Dr. Marcus Judge
- 14226

