By Dr. Keertana Anne and Dr. Tom Bradley
Next Lesson - Anaemia
Abstract
- Full blood counts are used very commonly in everyday practice to determine if patients have any haematological abnormalities.
- They are a set list of routine tests testing every part of the blood performed on one blood sample using an analyser.
- Blood films are made and used by biomedical scientists to view the blood cells and identify any abnormalities in terms of cells shape, size and number.
Core
Put simply, an abnormal result is one which falls outside the normal range of values or is drastically different to a previous result.
A normal range is a set of values within which a healthy patient should fall (for normal ranges, please refer to Figure 1. NB that normal ranges can vary between laboratories).
However, a normal range is by no means a perfect measure. The normal range will only include values for 95% of the normal healthy population. Therefore, 2.5% of the population will lie outside of the normal range without any pathology.
Therefore it is extremely important to not be blinkered by any blood tests. Blood tests should only be used as an adjunct to a good history and examination and should always be interpreted in the clinical context of the patient and in relation to any previous blood results.
The normal range also changes for different populations, and can be affected by; age, sex, ethnicity and co-morbidities.
A blood result may be abnormal if it shows a large change as blood values should not usually change physiologically.
If a result is unexpected the blood test should always be repeated as there are several sources of errors in processing a FBC:
Specimen collection error:
- There could be the wrong blood in the tube (blood is not that of the patient identified on the label).
- The wrong bottle could be used for the test(different bottles are required for different samples as they contain specific agents for that test).
- There could be pooling of different samples (repeated venepuncture to get a full tube).
- Poor technique or heavy handling of the sample can trigger the clotting cascade in the blood and alter the values affecting accuracy.
Delivery of specimen to laboratory error:
- The specimen can be delayed, not delivered or lost. An FBC should be processed within a timeframe specified by the local laboratory, as stability depends on storage conditions and the analyser used.
- The specimen can be delivered by the wrong method. Some samples need to be delivered at certain temperatures while others need to be hand delivered (as the sample can be damaged) rather than by pneumatic tube like most samples.
Specimen analysis and result reporting error:
- Specimen mix up can occur at the lab due to human error.
- Incorrect clinical details can be recorded due to poor handwriting being misread, or incorrect information being written down.
- The wrong test requested or performed.
- There is inherent test variability for the analysers as they are not 100% accurate all of the time.
- Technical errors can occur with the analysers.
Responsive action error:
- Sometimes nothing is done in response to an abnormal result.
- Reflex tests (extra tests required in response to the results of the FBC) are not carried out.
- The right result is applied to the wrong patient.
A FBC is measured using an automated test with a very high level of accuracy that uses an analysing machine that can process thousands of samples every day.
The sample must be placed and mixed in a tube containing k-EDTA. The k-EDTA acts to chelate calcium ions to prevent clotting, which would render the sample unusable. Never use a k-EDTA FBC tube to take a sample for urea and electrolyte (U&E) analysis. The potassium ion salt will provide an extremely high incorrect potassium value.
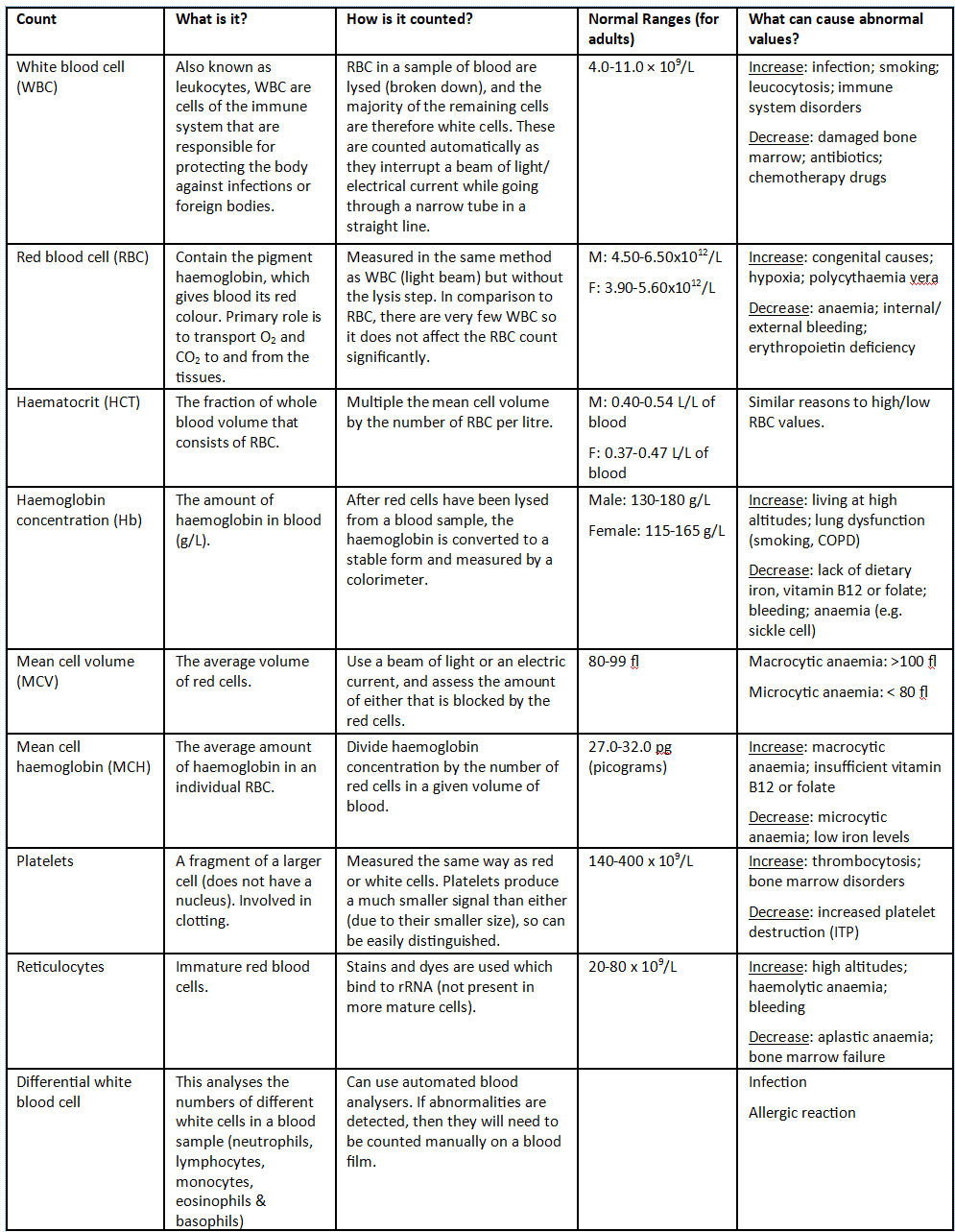
Figure 1: Shows what a FBC looks at, the normal ranges and what can cause it to increase or decrease
SimpleMed original by Dr. Keertana Anne and Dr. Tom Bradley
Samples with significant results outside of the normal range, significant change within the normal and abnormal (either immature or unable to identify) cells highlighted by the analyser are identified and a blood film is carried out.
To create a blood film:
- A drop of the patient’s blood is placed onto a glass slide and spread until it is a layer only one cell thick. This allows the cells to be viewed much more clearly as they are not being distorted by cells on-top of or below the red blood cells which are being observed.
- Fix the film with methanol to preserve cellular morphology for staining and to reduce biohazard risk to the observer.
- Stain the film with a Romanowsky-type stain (such as Wright or Giemsa), which contains methylene blue derivatives and eosin, to enable clear visualisation under the microscope.
Biomedical scientists review the blood film and any previous haematological results for that patient. If there are areas of concern, the blood film is then passed on to a haematologist for review and to add any medical comments or additional tests that may be required.
Terminology Used for Describing Red Blood Cells
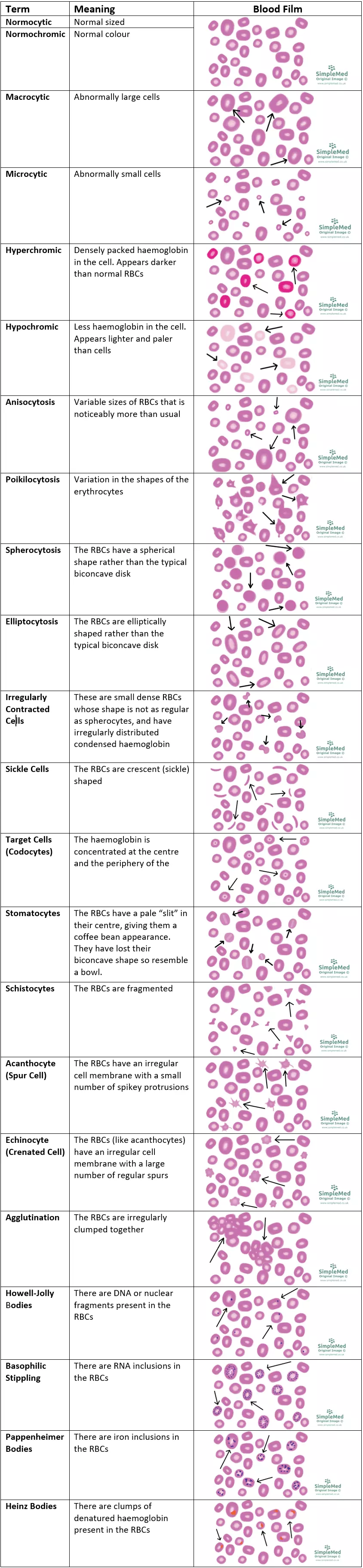
Figure 2: Different types of cells seen in blood films
SimpleMed original by Dr. Keertana Anne and Dr. Tom Bradley. All individual blood films hand drawn by Dr. Tom Bradley and Dr. Keertana Anne.
Edited by: Dr. Ben Appleby
Reviewed by: Dr. Thomas Burnell
- 15315

