By Dr. Sachin Sudhakaran and Dr. Maddie Swannack
Next Lesson - The Skull
Abstract
- Causes of midline neck lumps commonly include congenital abnormalities that cause collections of fluids, like dermoid cysts or thyroglossal duct cysts, or pathology of the thyroid gland. They can be differentiated on examination because thyroglossal duct cysts will move superiorly on tongue protrusion, and thyroid swellings will move superiorly on swallowing. Dermoid cysts will also show variations in cell type on USS.
- Causes of lateral neck lumps include lymph node swelling, which can be due to infection or malignancy, swelling of the salivary glands, which will cause pain on eating, branchial cysts and pathology of the carotid arteries, which will be pulsating.
- When seeing a patient presenting with a neck lump it is important to get a thorough history, and to screen for red flag symptoms.
- Investigation is done initially through ultrasound scanning, with fine needle aspiration if indicated. Progression to CT or MRI can be used.
Core
Due to the large number of structures in the neck, the differentials for neck lumps can be very varied. This article will give an overview of possible causes of neck lumps, and give some key features of neck lumps to ask about when attempting diagnosis of neck lumps in primary care.
To make it easier, this article is split into two parts. The first is a summary of the things that can cause a midline neck lump, that is to say a lump in the centre of the anterior neck. The second is a summary of the things that can cause a lump that is more lateral, so any lump that does not fall in the centre of the anterior neck.
A dermoid cyst is a congenital cystic teratoma that typically presents in the midline of the neck, often in the submental region. As this type of cyst is a teratoma, it can contain hair, teeth or skin glands alongside the fluid. They are generally painless.
A thyroglossal duct cyst is a congenital filled sac that forms in the midline of the neck. When the thyroid forms, it descends from the base of the tongue into the neck, leaving a path called the thyroglossal duct. Normally this completely obliterates, but in some people, it can remain patent, creating cavities that can fill with fluid.
The cysts are generally painless, and will move superiorly with protrusion of the tongue (because the tongue and the thyroid are connected with this patent duct). If the fluid in the cyst becomes infected, the cyst may become painful.
Standard treatment of thyroglossal duct cysts is surgical removal of the cyst and the entire thyroglossal duct. To reduce recurrence, this usually involves removal of the central portion of the hyoid bone along with the cyst and duct.
Pathology of the Thyroid Gland
The thyroid gland sits on the anterior trachea, just below the thyroid cartilage (‘Adam’s Apple’). This means that any swelling of the thyroid gland is very visible on the anterior neck, and (as previously mentioned) will move on swallowing as the thyroid is connected to the trachea.
Swellings of the thyroid can be benign (for example as a result of an autoimmune condition like Graves Disease) or malignant (papillary or follicular).
Lymph nodes are an important part of the lymphatic system and act as a physical and phagocytic filter. There are two classifications of lymph node in the neck.
Superficial Cervical Lymph Nodes
Superficial cervical lymph nodes are found within the superficial cervical fascia. Lymph from the face and scalp ultimately drain into these nodes, allowing for localised investigation into causes of lymphadenopathy (e.g. submental lymphadenopathy should prompt examination of the oral cavity).
Key superficial cervical lymph nodes
- Submental
- Submandibular
- Pre-auricular
- Post-auricular
- Occipital
- Superficial Cervical
- Posterior Cervical
- Anterior Cervical
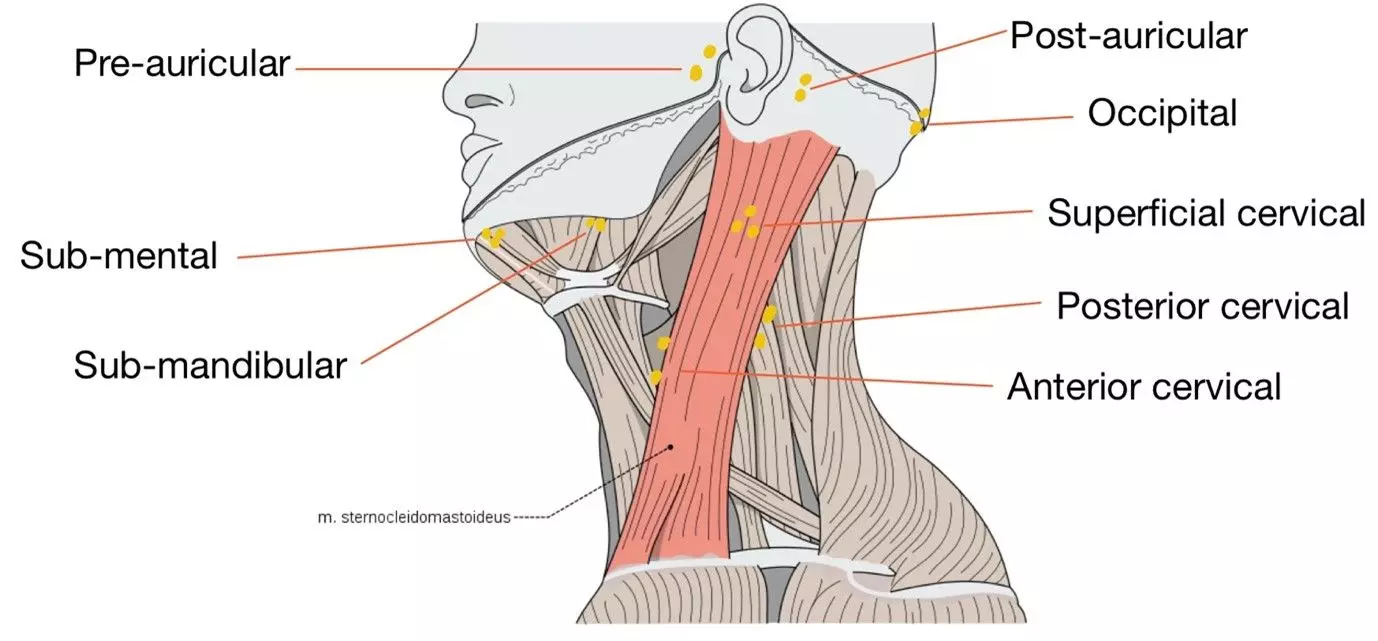
Diagram - Location of superficial lymph nodes on the left side of the head and neck
Creative commons source by Olek Remesz, edited by Dr. Sachin Sudhakaran [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Deep cervical lymph nodes are located deep to the superficial cervical fascia. They are closely associated with the internal jugular vein and can be found within the carotid sheath. Most superficial lymph nodes of the neck drain into these lymph nodes, and structures such as the thyroid and palatine tonsils drain directly into deep cervical lymph nodes. These lymph nodes are not usually palpable unless they are significantly enlarged.
Key deep cervical lymph nodes:
- Jugulo-digastric
- Jugulo-omohyoid
- Supraclavicular Lymph Nodes
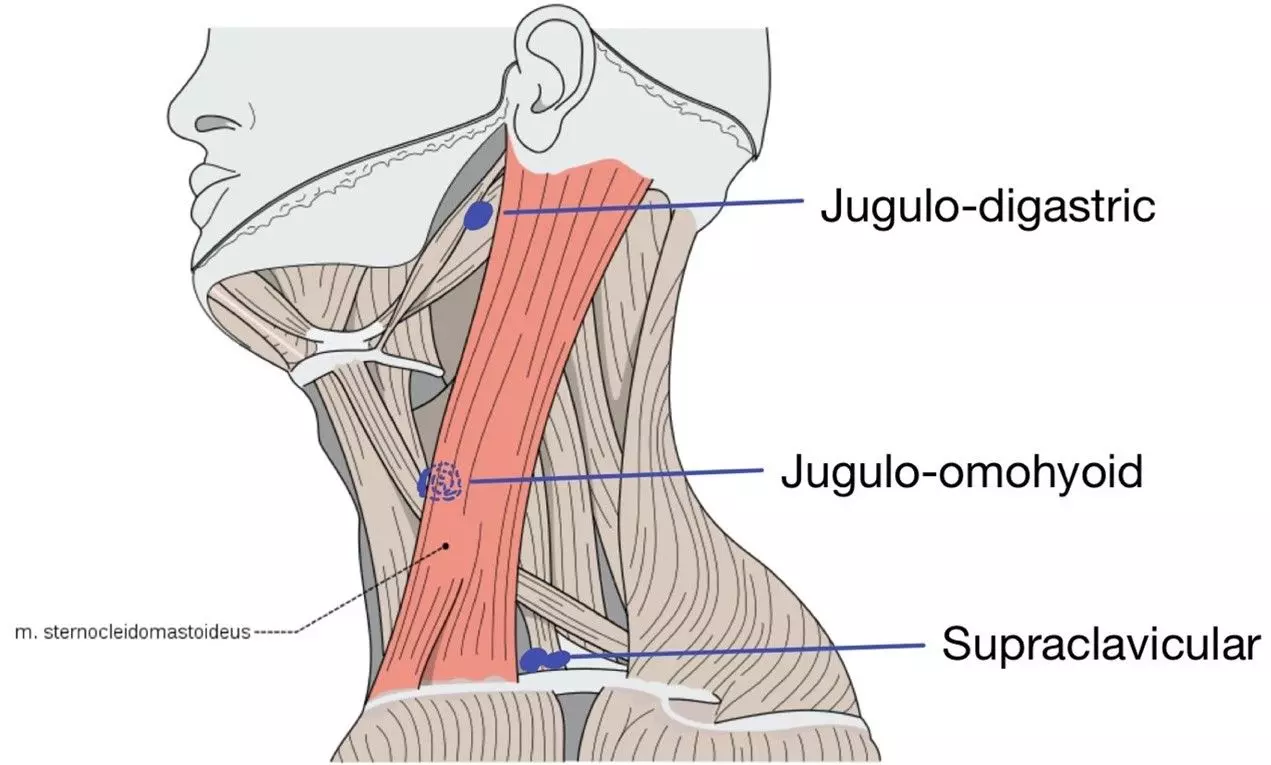
Diagram - Location of deep lymph nodes on the left side of the neck. Note that the supraclavicular nodes are usually found deep within the supraclavicular fossa
Creative commons source by Olek Remesz, edited by Dr. Sachin Sudhakaran [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Lymphadenopathy, or the swelling of lymph nodes, can occur for a number of reasons.
Lymph nodes can become swollen due to malignancy. This can be primary malignancy of the lymphatic system, such as lymphoma, or secondary malignancy causing swelling as cancer originating in another organ spreads to the lymphatic system.
One notable example of malignancy spreading to the lymph nodes in the neck is the left supraclavicular node, named Virchow’s Node, which is a sign of cancer in the abdominal cavity. This includes the stomach, ovaries, testicles and kidneys. As these cancers can remain asymptomatic while metastasising, it is important to examine for the lymphatic spread in the left supraclavicular fossa.
Lymphadenopathy can also occur as a result of infection. This is known as reactive lymphadenopathy, and these lymph nodes can be tender when examined.
The salivary glands that cause neck lumps are the submandibular (antero-inferior to the angle of the mandible) or the parotid (posterior to the angle of the mandible) glands. This means that any neck lumps caused by salivary glands are very lateral in their positioning.
Pathology of the salivary glands that can cause neck lumps includes calculi, infection or malignancy. The first two will be painful, especially on eating, but a malignancy may present painlessly.
A branchial cyst is a congenital cyst forming on the anterior superior portion of the sternocleidomastoid muscle of the neck.
Branchial cysts originate from the incomplete obliteration of the branchial arches, key features in the embryological formation of structures in the head and neck. Normally, the surfaces of the arches fuse, but in some cases, small gaps can be left unfused, which can form collections of fluid. Although normally painless, this fluid can become infected, making the lump painful.
Pathology of the Carotid Arteries
The carotid arteries are also a key structure in the neck. Pathology of the carotid arteries can include aneurysms or tumours (paragangliomas), which would be along the course of the carotid artery and would be pulsating. Auscultation of the lump would reveal a bruit.
There are numerous causes for neck lumps, spanning from recent or concurrent infection to underlying malignancy. To add another level of complexity, neck lumps may not be associated with lymph nodes at all. When presented with a neck lump, it’s important to perform a thorough history and examination.
Factors to explore in the history:
- Age
- Duration
- Progression - e.g. change in size, texture, temperature.
- Consider associated symptoms - e.g. sore throat, change in voice, difficulty breathing, difficulty swallowing.
- Explore red flag symptoms (see below)
Key features on examination:
- General inspection - e.g. scars, hoarseness of voice, exophthalmos.
- Location - is it in the midline or is it in the anterior or posterior triangle of the neck?
- If midline:
- Ask the patient to swallow some water to assess movement of the mass (movement upwards during swallowing is suggestive of a thyroid mass due to the thyroid’s attachment to the trachea).
- Ask the patient to protrude their tongue (with thyroglossal duct cysts, the lump moves upwards).
- Palpate and identify:
- Size
- Shape - are there identifiable borders?
- Consistency - is it hard, soft, smooth, irregular?
- Mobility - is it tethered to surrounding tissue?
- Tenderness
- Overlying skin changes (e.g. erythema)
Important Red Flags:
- Present for more than 6 weeks
- Hard and irregular texture
- Fixed/tethered to surrounding tissue
- Rapidly growing in size
- Associated fatigue, weight loss, night sweats
- Associated hoarseness or dysphagia
Neck lumps are commonly investigated with an ultrasound scan (USS). This allows for further identification of the lump. If a lump is suspicious on USS, an ultrasound-guided fine needle aspiration is usually indicated.
If further imaging is required, CT or MRI scans may be offered, especially if surgical management may be needed.
Reviewed by: Dr. Thomas Burnell
- 8346

