By Dr. Sachin Sudhakaran and Dr. Maddie Swannack
Next Lesson - Cranial Nerves VII-XII
Abstract
- There are a total of 12 pairs of cranial nerves extending from the brain/brain stem. There are 2 arising from the brain, 2 from the mid brain, 4 from the pons and 4 from the medulla.
- The cranial nerves have unique motor, general sensory and special sensory functions. Cranial Nerves may have a function which is purely motor, purely sensory, special sensory or a combination.
- The olfactory nerve has a special sensory function in facilitating the sense of smell (olfaction).
- The optic nerve has a special sensory function in facilitating the sense of vision.
- The oculomotor, trochlear and abducens nerves supply motor innervation to muscles within the orbit to control the movements of the eye.
- The trigeminal nerve supplies sensation to the face, and motor innervation to the muscles of mastication.
Core
Introduction to Cranial Nerves
The cranial nerves are 12 pairs of nerves which arise from the brain and have various motor, sensory, special sensory and autonomic functions.
For clarity a special sensory function is any sense other than touch specifically vision, taste, smell, hearing and balance.
The 12 cranial nerves and their functions are as follows. Helpful tips for remembering these are shown in the blue columns:
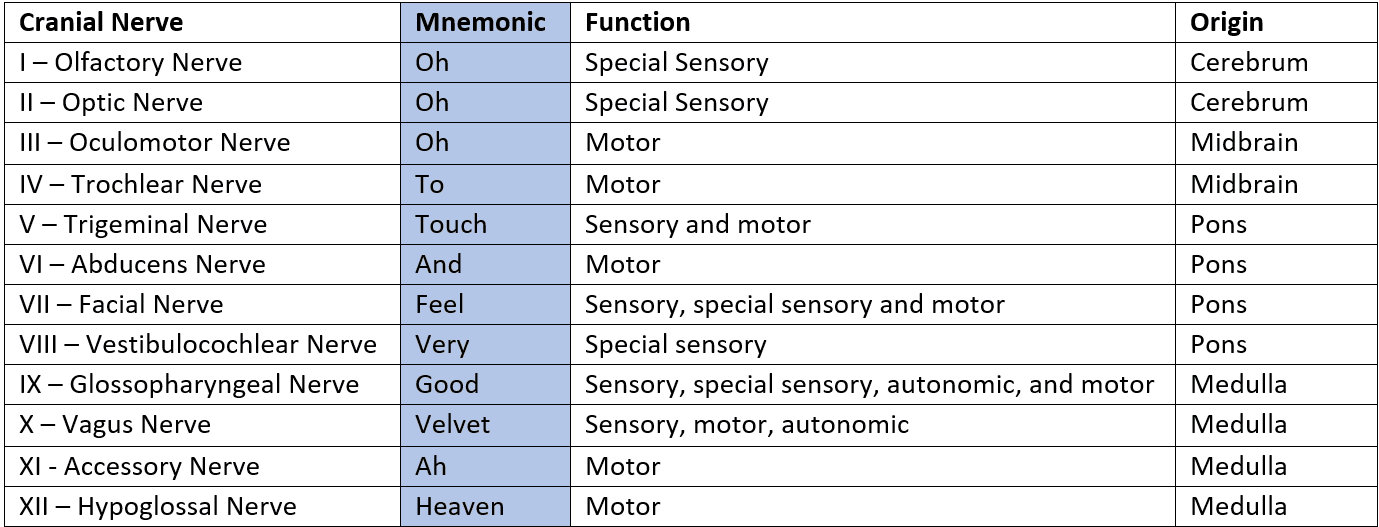
Table - The origin and functions of the 12 cranial nerves
SimpleMed Original by Dr. Sachin Sudhakaran
The image below shows the anatomical origins of the cranial nerves.
The first 2 nerves emerge from the cerebrum - olfactory and optic.
The next 2 nerves emerge from the midbrain - oculomotor and trochlear.
The next 4 nerves emerge from the pons - trigeminal, abducens, facial and vestibulocochlear.
The final 4 nerves emerge from the medulla - glossopharyngeal, vagus, accessory and hypoglossal.
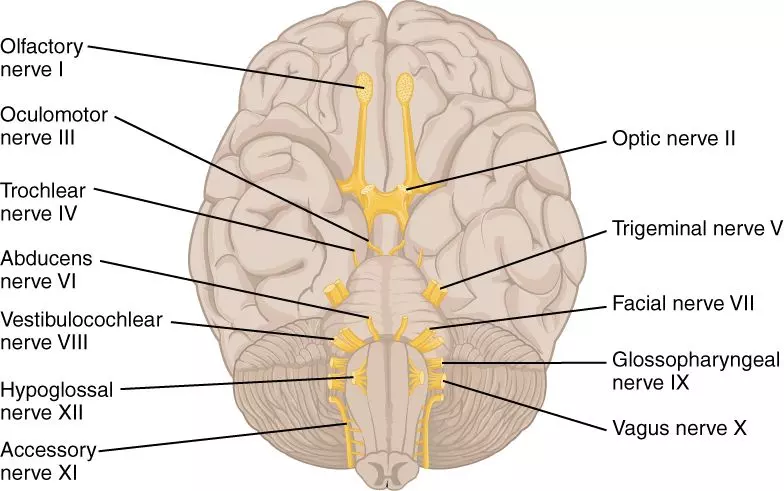
Diagram - Illustration indicating the origin of all 12 cranial nerves
Creative commons source by OpenStax [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
This article will cover the path and function of the first six cranial nerves.
Function
These nerves are used in providing the sense of smell (olfaction).
Pathway
Found at the roof of the nasal cavity, fibres from the olfactory nerve pass through the cribriform foramina (literally ‘sieve holes’) of the cribriform plate. This plate is a feature of the ethmoid bone of the skull.
Once inside the skull, these nerve fibres coalesce to form the olfactory bulb. From the olfactory bulb the fibres travel as a single nerve called the olfactory tract which extends to the temporal lobe of the brain.
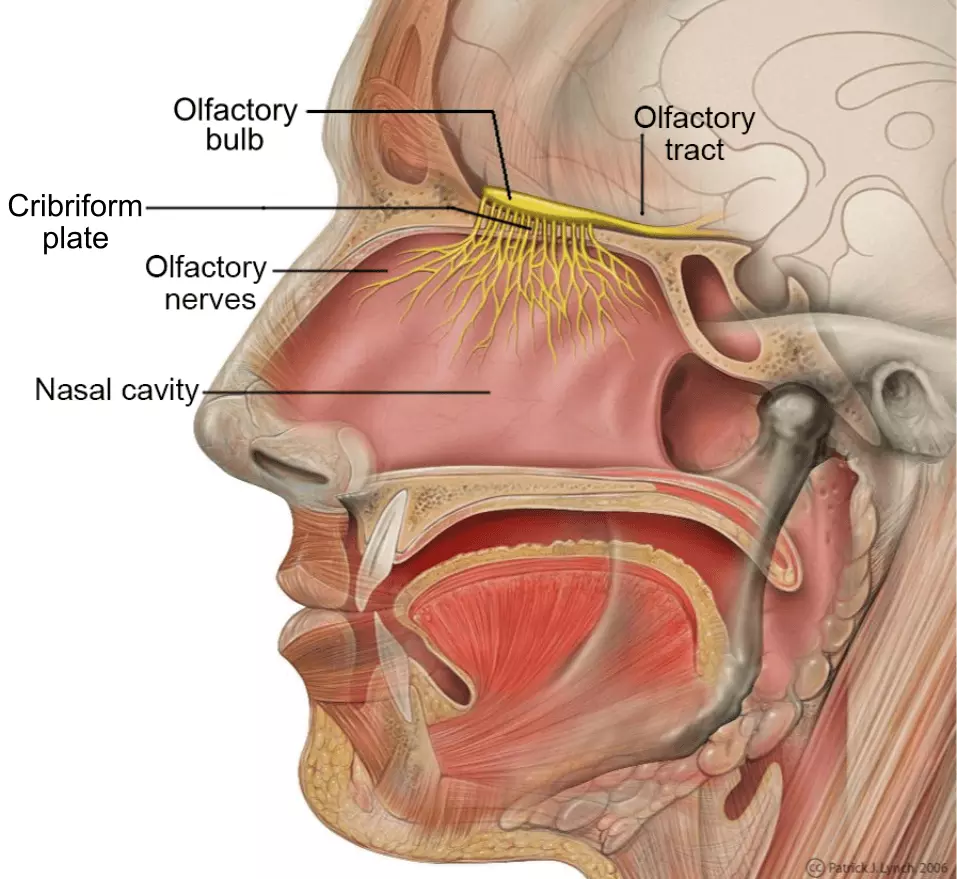
Diagram - Illustration showcasing the path of the olfactory nerve from the roof of the nasal cavity. Remember that the olfactory tract extends posteriorly to the temporal lobe
Creative commons source by Patrick J. Lynch [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Pathology
Pathology of this nerve is usually the result of external compression or sudden trauma to the nerve, such as a fracture of the ethmoid bone caused by a road traffic accident. Affected patients will report a loss of smell (anosmia).
Testing
To test this nerve, ask the patient about any change in their sense of smell and, where appropriate, test each nostril separately using a familiar, non-irritant odour.
Function
These nerves are used in providing the sense of vision.
Pathway
Very simply put, when light enters the eye and hits the photoreceptor cells of the retina, graded electrical signals are generated which ultimately lead to action potentials in the retinal ganglion cells. The action potential is carried along the optic nerve to the visual cortex of the brain where it is interpreted as vision. The nerve is communicated via the optic canal in the sphenoid bone.
To properly understand how the optic nerves of a patient are functioning it is important to understand the concept of visual fields.
Visual Fields
When describing the eye, the terms temporal (closer to the temporal bone, lateral) and nasal (closer to the nose, medial) are used in place of lateral and medial. The visual fields are also divided into 4 quadrants. Visual fields describe the orientation of objects in the patient’s vision and retina where the light from those objects is detected.
When light enters the eye, it will strike the contralateral side of the retina. As shown in the diagram below, light from an object to the side of the patient (temporal vision) will hit the nasal surface of the retina, and vice versa.
To further complicate things the same occurs with light coming from above or below the patient. Light coming from above the patient will hit the inferior surface of the retina, and vice versa.
In summary light from an object in the inferior temporal visual field will hit the superior nasal visual field.
This does not mean that we perceive the world upside down or back to front as the brain corrects for this effect. Nevertheless, it is an important fact to keep in mind when assessing for lesions along the visual pathways.
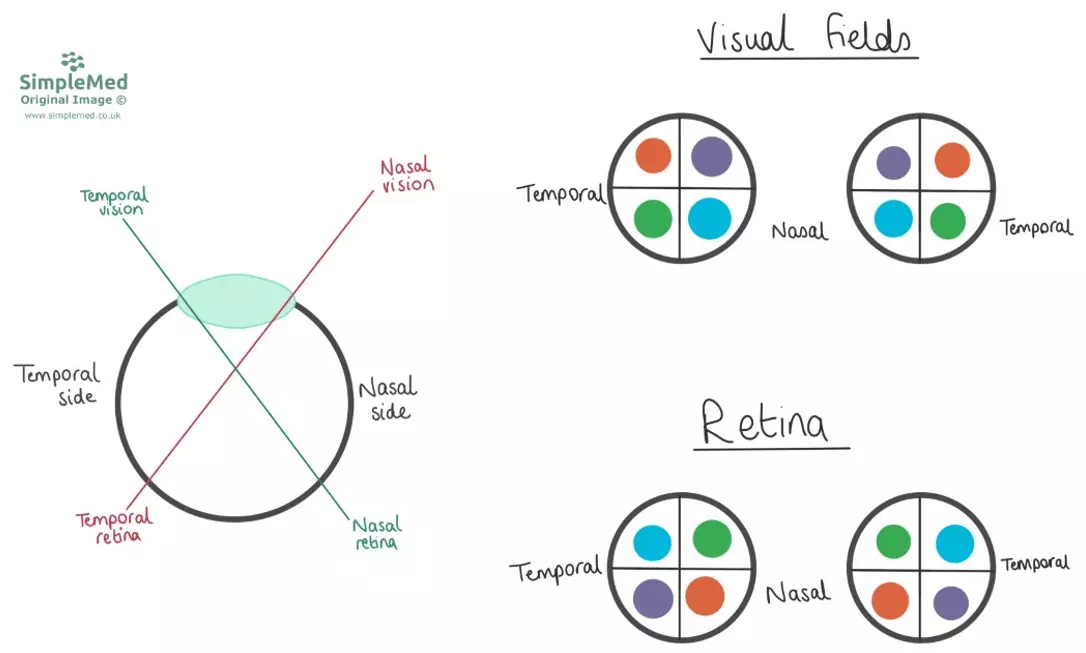
Diagram - How light enters the eye and hits the contralateral side of the retina, and how this leads to the visual fields corresponding to the retinal areas (with the same areas shown in the same colours), e.g. the orange object is above and lateral to the patient, but the image is seen on the inferior nasal quadrant
SimpleMed original by Dr. Maddie Swannack
Once the optic nerve fibres on the surface of the retina converge to form the optic nerve they travel posteriorly and converge to form the optic chiasm. At this chiasm, the axons converge, with fibres from the nasal retina decussating (swapping sides) and fibres from the temporal retina remaining on the same side. Exiting this chiasm are the optic tracts. The tracts will carry images from the ipsilateral temporal retinal image and the contralateral nasal image (from the other side), i.e. the left optic tract will carry all the information from the left side of both retinas which is from the right temporal field. This is shown in the image below.
Diagram - The pathway of the visual system
Creative commons source by Wiley [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The optic tracts extend to the lateral geniculate nuclei in the thalamus. From here, two optic radiations are projected from each optic tract, which extend to the primary visual cortex in the occipital lobe.
There are two radiations - the superior optic radiations which travel through the parietal lobes and the inferior optic radiations which travel through the temporal lobes. The superior tracts carry all the information from the superior retina and thus all the images from the inferior half of vision.
Likewise the inferior tracts carry all the information from the inferior retina and thus all the images from the superior half of vision.
Pathology
Lesions of the visual tract give different patterns of visual loss depending on the site (e.g. direct compression of the optic chiasm by a pituitary tumour could cause bitemporal hemianopia). This will be covered more in the Neuroanatomy Unit.
Testing
Visual acuity tests are used to test the optic nerve, e.g. Snellen charts, checking pupillary responses to light, and checking visual fields.
It’s equally important to visualise the retina through fundoscopy by using an ophthalmoscope.
Movement of the Eyeball - Cranial Nerves III, IV and VI
Primary Functions
There are six muscles that control movement of the eyeball. The four easiest to understand are called superior rectus, inferior rectus, medial rectus and lateral rectus. When they contract, they pull the eyeball in the direction of their name e.g. the superior rectus moves the eye superiorly (looking upwards).
The two remaining muscles are called the superior oblique and inferior oblique. These muscles attach to the eye at an oblique angle. As a result, when they contract, they rotate the eyeball. This means that superior oblique is responsible for the intorsion (internal rotation) of the eyeball, and inferior oblique is responsible for the extortion of the eyeball. This movement is key in keeping the visual image stable when the head is tilted to the side.
All the muscles work antagonistically to each other to keep the eye in position. If a muscle loses its tone, the other muscles will pull away from it and move the eye out of position e.g. if the superior rectus is weak, the eye will be pulled inferiorly.
These are all shown in the diagram below:
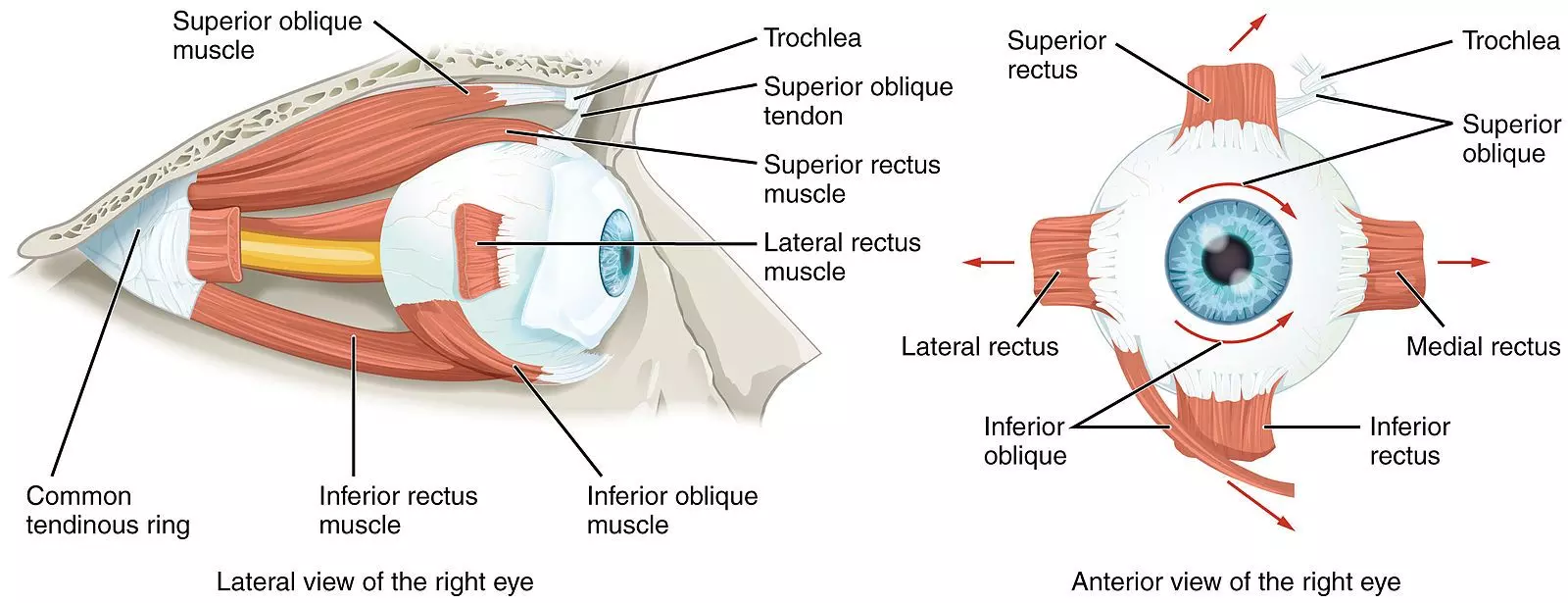
Diagram - The extra-ocular muscles of the right eye. Note the oblique paths of the superior and inferior oblique muscles
Creative commons source by OpenStax College [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Secondary Functions
Some of the muscles also have secondary directions of pull, shown in the table below:
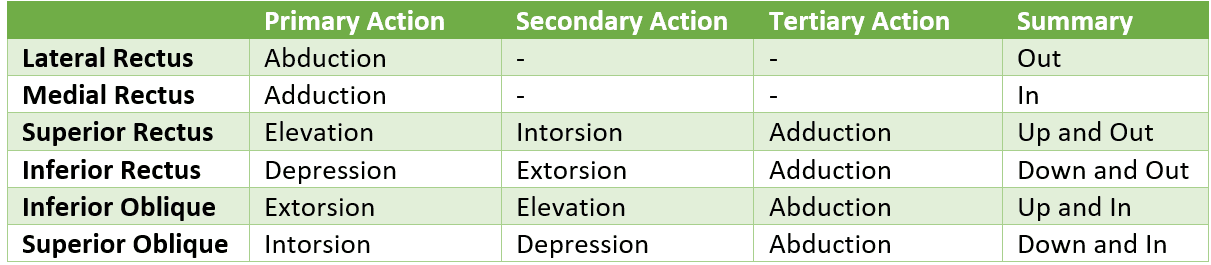
Table - The secondary functions of the extraocular muscles
This table can be quite complicated - the important thing to remember is the primary function.
Also remember that if the function of a muscle is lost, the eye will move in the opposite direction because the pull of the other muscles is unopposed.
Innervations
The six muscles which move the eye are innervated by one of three cranial nerves.
- Superior Rectus - Oculomotor (III)
- Superior Oblique - Trochlear (IV)
- Medial Rectus - Oculomotor (III)
- Inferior Rectus - Oculomotor (III)
- Inferior Oblique - Oculomotor (III)
- Lateral Rectus - Abducens (VI), so called as the lateral rectus abducts the eye
Which muscle innervates which muscle is difficult to remember. The mnemonic ‘LR6 SO4’ may act as an aid. This will help with knowing that the lateral rectus is innervated by cranial nerve VI (abducens) and that superior oblique is innervated by cranial nerve IV (trochlear). The rest are innervated by cranial nerve III (oculomotor).
Cranial Nerve III - Oculomotor
Function
The oculomotor nerve innervates four of the extra-ocular muscles (listed above and shown in image below) in addition to levator palpebrae superioris (responsible for elevating the eyelid) and sphincter pupillae (constricts the pupil). It also carries autonomic parasympathetic fibres.
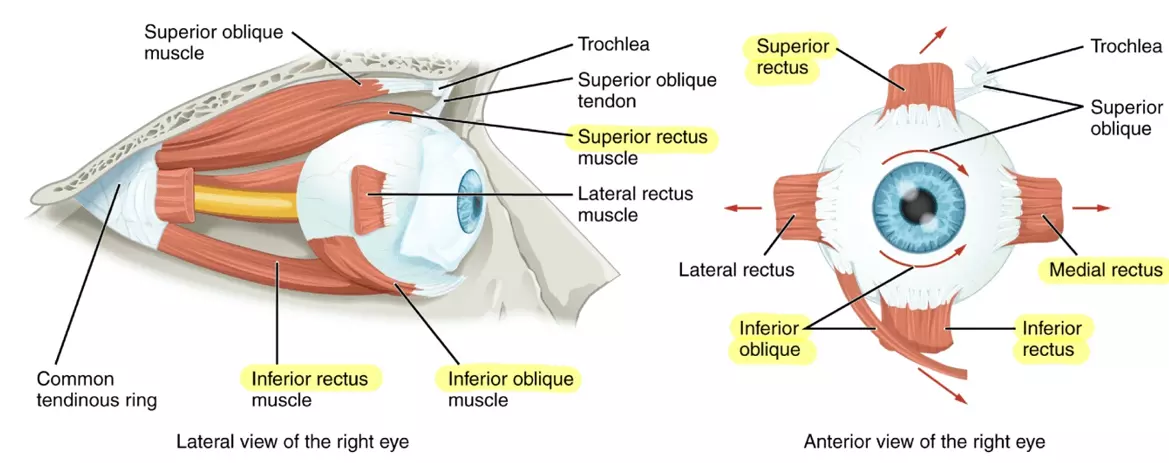
Diagram - The extraocular muscles of the eye. The highlighted muscles are innervated by the oculomotor nerve
Creative commons source by OpenStax College, edited by Dr. Sachin Sudhakaran [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Pathway
Originating from the midbrain, fibres from the oculomotor nerve travel through the cavernous sinus, through the superior orbital fissure to innervate its respective muscles.
Pathology
Pathology of this nerve is usually the result of external compression. This can be due to a number of causes including raised intracranial pressure, aneurysms and cavernous sinus thrombosis.
Patients with pathology of this nerve usually have diplopia (double vision) and severe ptosis (drooping of the upper eyelid) due to loss of innervation to the levator palpebrae superioris muscle, and may have a dilated (blown) pupil due to loss of parasympathetic impulses to the sphincter pupillae muscle.
The patient will present with the affected eye in a ‘down and out’ position (lateral and inferior) due to the paralysis of four of the extra-ocular muscles. This leaves only lateral rectus and superior oblique functioning, pulling the eye laterally and inferiorly.

Image - Patient presenting with a ‘down and out’ position of the left eye. Notice how the eyelids have to be retracted, this is most likely due to ptosis of the left eye secondary to an oculomotor nerve lesion
Creative commons source by Wang Y, Wang XH, Tian MM, Xie CJ, Liu Y, Pan QQ, Lu YN [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Testing
To test this nerve:
- Inspect the eyelids and pupils (check for asymmetry)
- Test the eye movements (using the H test - see below)
- Test the pupillary reflexes
Function
A nerve with purely motor function, this nerve innervates the superior oblique muscle, which primarily intorts and depresses the eye, particularly when the eye is adducted.
Pathway
Originating from the dorsal aspect of the midbrain, this nerve passes through the cavernous sinus and superior orbital fissure before innervating the superior oblique muscle. This nerve has the longest intracranial length of the cranial nerves.
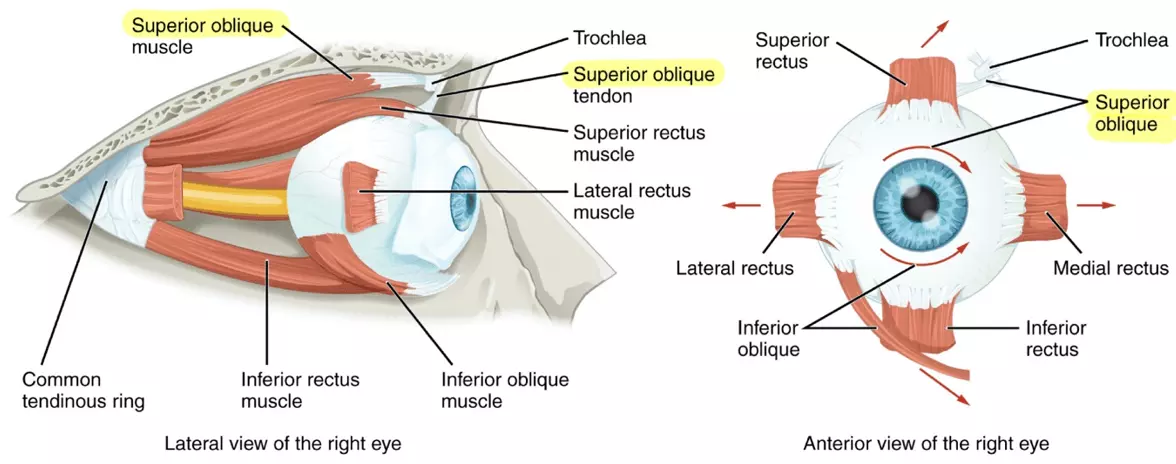
Diagram - The extra-ocular muscles of the eye. The highlighted muscles are innervated by the trochlear nerve
Creative commons source by OpenStax College [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Pathology
Pathology is usually the result of raised intracranial pressure. The nerve is very susceptible to pressure as a result of its long intracranial length.
Patients with trochlear nerve palsies will complain of a downward gaze diplopia (double vision that is worse when looking down, e.g. when reading or walking downstairs). This is because the affected eye has a weakness in looking down, so will not be able to follow the functional eye to the inferior position.
The eye may appear slightly elevated and extorted because the depression and intorsion actions of the superior oblique are lost, particularly when the eye is adducted.
Testing
Test this nerve by testing eye movements (using the H test - see later).
Function
This nerve also only has one motor function: it innervates the lateral rectus of the eye, which is involved in abducting the eye.
Pathway
Arising from the pons, it passes through both the cavernous sinus and the superior orbital fissure before innervating the lateral rectus muscle.
Pathology
Patients with pathology of the abducens present with diplopia usually due to compression against the pons from raised intracranial pressure.
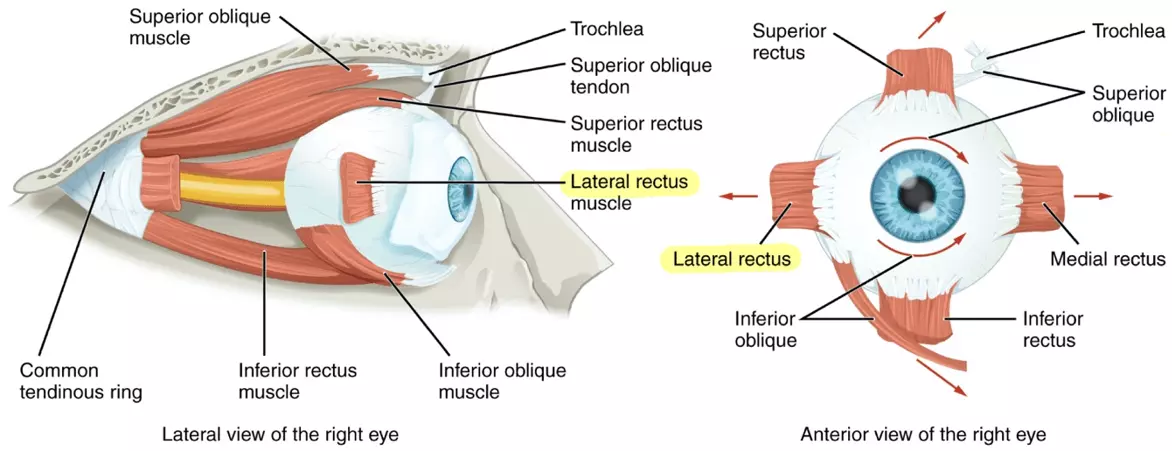
Diagram - Extra-ocular muscles of the eye. Highlighted muscles are innervated by the abducens
Creative commons source by OpenStax College [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Testing
To test this nerve, test the eye movements (using the H test).
All three nerves that control eye movement can be tested through one test, called the H test.
The test is conducted by having the patient keep their head still and to follow the movements of a finger or pen. The aim is to evaluate the activity of specific eye muscles by performing movements which isolate their action.
Performing the H Test
First, set the patient up with their eyes in a neutral position. Ask the patient to follow your finger or pen with their eyes whilst keeping their head still to isolate the movements of the muscles of the eye. Ask the patient to report if they see double at any point. If the patient usually wears spectacles for this test ensure they are worn.
For clarity, this example details the muscles of the left eye during the test (see diagram below), however, when carrying out the test both eyes are observed simultaneously.
Move the pen to the left side of the patient’s head (lateral to the left eye) to abduct the left eye. This tests the function of the lateral rectus muscle, and therefore the abducens nerve (VI).
Next move the pen superiorly. This tests the function of the superior rectus muscle and therefore the oculomotor (III) nerve.
Still on the left side of the patient’s head, move inferiorly. This tests the function of the inferior rectus and therefore the oculomotor (III) nerve.
Return to the centre on the left side. Slowly move the pen across the centre of the vision to the right side of the head medial to the left eye to adduct the left eye. This tests the function of the medial rectus and therefore the oculomotor (III) nerve.
Next, move superiorly. This tests the function of the inferior oblique muscle and therefore the oculomotor (III) nerve.
Still on the right side, move inferiorly. This tests the function of the superior oblique muscle and therefore the trochlear (IV) nerve.
By the end of the test your pen should have traced an ‘H’ in the air in front of the patient’s face.
This test can be difficult to describe in words, so refer to the diagram below for clarification.
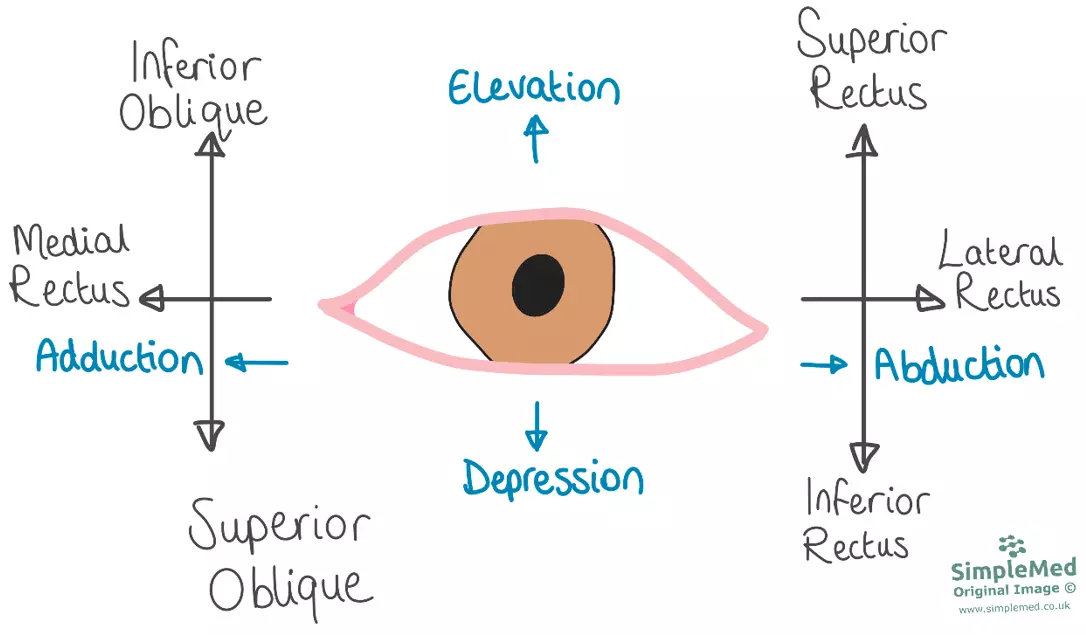
Diagram - The muscles involved in the ‘H Test’ when performed on the left eye. Eye movements tested are listed in blue, and the muscles that are isolated by performing that movement are shown on the ends of the ‘H’
SimpleMed original by Dr. Maddie Swannack
Function
The trigeminal nerve supplies sensory function to the face. It also supplies the muscles of mastication.
Pathway
Arising from the pons, this nerve splits into 3 branches at the trigeminal ganglion:
Ophthalmic Branch (Cranial Nerve Va)
Passing through the cavernous sinus and the superior orbital fissure, this nerve provides general sensation to the forehead, eye and nose.
This nerve also provides the afferent (sensory) fibres for the corneal reflex, the involuntary blink reflex that occurs when the cornea is touched. The efferent (motor) fibres that control the eyelids are innervated by the facial nerve (VII).
Maxillary Branch (Cranial Nerve Vb)
Passing through foramen rotundum via the cavernous sinus, this nerve splits into two further branches:
- Superior Alveolar - provides sensation to the upper teeth and gums.
- Infraorbital - provides sensation to the cheeks, lower eyelid and upper lip.
Mandibular Branch (Cranial Nerve Vc)
Unlike the previous two branches, this nerve does not pass through the cavernous sinus. Rather, it passes through the foramen ovale into the infratemporal fossa to split into three branches:
- Inferior Alveolar - this branch enters the mandibular canal and emerges through the mental foramen as the mental nerve, providing sensation to the lower lip and chin.
- Lingual - providing general sensation to the anterior 2/3 of the tongue.
- Auriculotemporal - providing general sensation to the temple, lateral side of the head and scalp, and the temporomandibular joint.
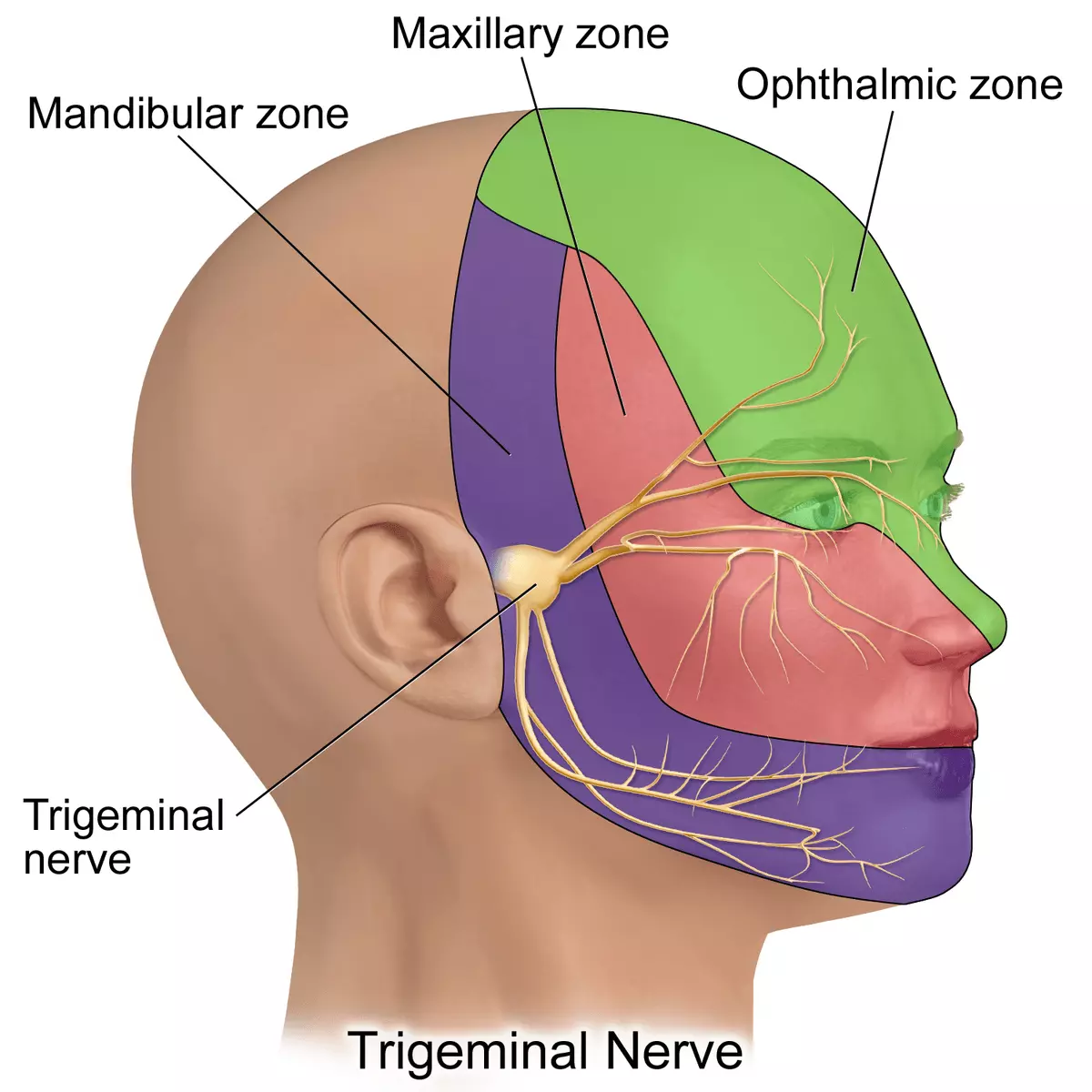
Diagram - The different areas of sensation provided by the different branches of the trigeminal nerve
Creative commons source by BruceBlaus [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Pathology
Trigeminal neuralgia is a condition involving compression and demyelination of the trigeminal nerve. It presents with excruciating pain on very light contact of the face, often described as electrical shocks, and due to the nature of the disease it can be difficult to manage.
Testing
This nerve is tested by examination of sensation to touch in areas innervated by each of its branches and may include testing the corneal reflex (although this is usually omitted due to its uncomfortable nature).
The motor function of the nerve is tested by palpation of the muscles of mastication whilst the jaw is clenched and asking the patient to move their jaw from side to side.
Edited by: Dr. Ben Appleby
Reviewed by: Dr. Thomas Burnell
- 21887

